
Here's a quick look at what we'll cover in this article:
Have you ever felt like you're moving through life while everyone else seems to be speaking a language you don't understand? That feeling of disconnection can be a part of living with depression, a common mood disorder that affects millions. Understanding the symptoms of depression is crucial for your mental health journey. This guide will help you recognize the signs in yourself and others, offering clarity on this complex condition and shedding light on the path to feeling better.
Depression is more than just having a bad day or a temporary low mood; it's a persistent mental illness that can impact every part of your life. This depressive disorder causes ongoing feelings of sadness and a loss of interest in activities you once enjoyed.
To receive a diagnosis of depression, symptoms must be present for at least two weeks. Understanding what depression is, how it differs from sadness, and its impact on both mind and body is the first step. Let's explore these key distinctions.
So, what exactly is this condition? Depression, also known as major depressive disorder, is a mood disorder that creates a persistent feeling of sadness and a significant loss of interest in daily life. It affects how you feel, think, and behave, leading to a range of emotional and physical problems. Unlike temporary sadness, it doesn't just go away.
This depressive disorder is one of the most common mental health conditions. It's characterized by symptoms that are severe enough to cause noticeable issues in your day-to-day activities, such as work, school, or social relationships. Some people may feel generally miserable without understanding why.
The good news is that depression is a treatable condition. With the right support and treatment, most people can find relief from their symptoms and regain their quality of life. Recognizing it is the essential first step toward recovery.
It's completely normal to feel sad in response to difficult life situations, like a breakup or losing a job. So, how is clinical depression different? The main distinction lies in persistence and pervasiveness. Everyday sadness is typically linked to a specific event and subsides with time. A depressed mood, however, is a key feature of this mood disorder and lasts for at least two weeks, affecting nearly every aspect of your life.
Depression involves more than just sadness. It comes with a cluster of other symptoms, such as a loss of interest in hobbies, changes in sleep or appetite, and persistent negative thoughts. While a person feeling sad can often be cheered up or find moments of enjoyment, someone with depression may find it difficult to experience pleasure at all.
Ultimately, depression isn't a weakness or something you can simply "snap out of." It's a serious medical condition that often requires professional treatment to improve.
Is depression all in your head, or does it affect your body too? The answer is both. While it's classified as a mental illness, depression has very real physical components. It's a complex condition that creates a powerful link between your mind and body, causing both emotional and physical symptoms.
From a biological standpoint, depression is associated with physical changes in the brain and an imbalance in brain chemistry. Neurotransmitters, which are chemicals that regulate mood, sleep, and appetite, are thought to play a significant role. This is why you might experience physical symptoms like fatigue, aches, and changes in weight.
Certain health conditions, such as thyroid problems, heart disease, and chronic pain, can also trigger or worsen depression. This highlights how interconnected your physical and mental health truly are. Therefore, treating depression often involves addressing both the mind and the body.

Recognizing the signs of depression is key to getting help. The symptoms can vary from person to person and range in severity. To be diagnosed with a major depressive episode, you generally must experience at least five specific depressive symptoms nearly every day for at least two weeks.
These symptoms of depression often fall into three main categories: emotional, physical, and behavioral. Understanding these different signs can help you identify if you or someone you know might be struggling. Let's look at each of these categories more closely.
The most well-known symptom of depression is a persistent depressed mood. This isn't just feeling sad; it can also manifest as a feeling of emptiness or hopelessness. For some, especially children and teens, it might look more like irritability or frequent anger outbursts over small things.
Another significant emotional sign is a loss of interest or pleasure in activities you once enjoyed, a symptom known as anhedonia. This could mean no longer enjoying hobbies, sports, or spending time with loved ones. You might also be plagued by negative thoughts and feelings of worthlessness or excessive guilt, often fixating on past failures.
In severe cases, these feelings can escalate to frequent or recurrent suicidal thoughts. Some of the core emotional signs include:
Depression doesn't just reside in your mind; it can have a profound impact on your body. Many people with depression experience significant physical symptoms that can be just as debilitating as the emotional ones. One of the most common is overwhelming fatigue and a lack of energy, where even small tasks feel like they require a huge effort.
Sleep patterns are also frequently disrupted. You might struggle with insomnia (trouble sleeping) or hypersomnia (sleeping too much). Appetite and weight changes are common as well, leading to either weight loss from a reduced appetite or weight gain from increased cravings for food. Some people also experience unexplained physical problems that can be linked to their mental state.
These physical manifestations can sometimes be a clue that something is wrong, even before the emotional symptoms are fully recognized. Physical symptoms may include:
When someone is struggling with depression, their behavior often changes in noticeable ways. Perhaps the most common behavioral change is social withdrawal. A person who was once social may start isolating themselves, wanting to stay home rather than go out and spend time with friends or family.
You might also notice changes in their daily functioning. This can include slowed thinking, speaking, or body movements. Conversely, some people may experience agitation and restlessness. To cope with their emotional pain, some individuals may turn to substance use, such as abusing alcohol or recreational drugs, which can worsen other mental health disorders.
These behavioral changes are often a direct result of the emotional and physical toll of depression. Key behavioral signs to watch for include:
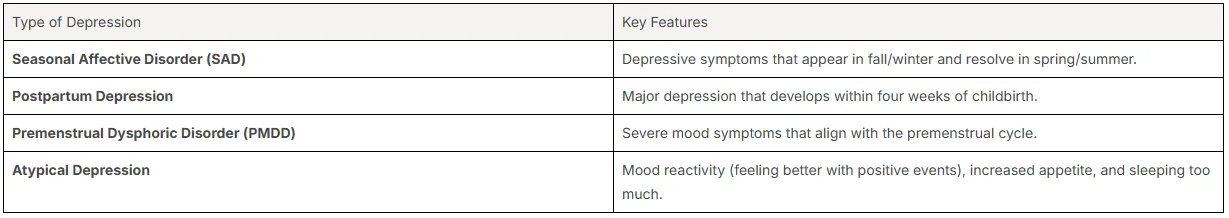
Did you know that depression isn't a one-size-fits-all condition? The American Psychiatric Association recognizes several different forms of depressive disorder. The specific type of depression is often determined by the context and pattern of your symptoms. Common diagnoses include major depression and persistent depressive disorder.
Other forms, like seasonal affective disorder, are linked to specific triggers or times of the year. Understanding the different types can help you find the most effective treatment. Let's explore some of the most common classifications of this mood disorder.
Major depressive disorder (MDD), often called clinical depression, is the most severe and common form. A diagnosis of MDD means you've experienced a depressed mood or loss of interest for at least two weeks, along with other depressive symptoms like sleep problems or fatigue. These episodes can be intense and significantly interfere with your ability to function.
On the other hand, there's persistent depressive disorder (PDD), previously known as dysthymia. PDD involves mild or moderate depression that is long-lasting, continuing for at least two years. The symptoms are less severe than those of major depressive disorder, but their chronic nature can still take a significant toll on your life.
While MDD is characterized by distinct, often severe episodes, PDD is more of a constant, low-level cloud of depression. It's possible for someone with PDD to also experience episodes of major depression.
Beyond major depression, several specific forms are linked to particular circumstances or symptom patterns. One well-known type is seasonal affective disorder (SAD), a form of major depression that typically occurs during the fall and winter months when there is less natural sunlight.
Other types are related to hormonal changes. Prenatal and postpartum depression occur during pregnancy or within four weeks of giving birth, respectively. Premenstrual dysphoric disorder (PMDD) involves severe depressive symptoms, irritability, and anxiety in the week or two before a period begins.
Atypical depression is another variant where mood can temporarily improve in response to positive events. It often includes symptoms like increased appetite and sensitivity to rejection.
Can you have depression and anxiety at the same time? Absolutely. It's very common for these two mental health disorders to occur together. Many people diagnosed with depression also experience symptoms of an anxiety disorder, such as excessive worry, nervousness, and restlessness. This combination can make symptoms of both conditions feel more intense.
The relationship between them is complex. Sometimes, one can trigger the other. For example, the social isolation that comes with depression can lead to social anxiety. In other cases, they may share common underlying causes, such as genetics or brain chemistry. Co-occurring depression and anxiety can also increase the risk for other issues, like substance use disorders.
Because they often overlap, treatment plans frequently address both conditions simultaneously. Therapies like cognitive behavioral therapy are effective for both, and some medications can help manage the symptoms of depression with anxiety. It's important to discuss all your symptoms with a healthcare provider to get the right diagnosis and care.
Why do some people develop depression while others don't? Researchers believe there isn't a single answer. Instead, the causes of depression are likely a combination of biological, genetic, and environmental factors. Your unique brain chemistry and family history can play a role, as can stressful experiences.
Certain risk factors, such as having other mental health conditions or chronic illnesses, can also increase your vulnerability. Understanding these influences can provide insight into why depression might develop. Let's look at some of the key biological and environmental triggers.
Your biology can play a significant part in your risk for depression. One of the key biological factors is brain chemistry. Imbalances in neurotransmitters, which are chemicals like serotonin and dopamine that help regulate mood, are thought to contribute to the development of this condition. This is why many antidepressants work by targeting these chemical pathways.
Genetic influences are also important. If you have a close blood relative, like a parent or sibling, with a history of depression, you are about three times more likely to develop it than someone with no family history. Researchers are actively working to identify the specific genes involved in causing mental disorders like depression.
Hormonal changes can also trigger depression. Fluctuations in hormones during pregnancy, after childbirth (postpartum), or due to conditions like thyroid problems or menopause can all contribute to the onset of depressive symptoms. These biological predispositions don't guarantee you'll get depression, but they do increase the risk.
While biology sets the stage, your environment and life experiences often act as triggers. Traumatic or stressful events can be powerful environmental triggers for depression. These can include physical or sexual abuse, the death of a loved one, a difficult relationship, or significant financial problems.
Certain lifestyle changes and choices can also contribute. For instance, the use of alcohol or other substances can cause depression or make it worse. A lack of social support and feelings of isolation can also increase vulnerability, making it harder to cope with challenging life events.
It's often a combination of these factors that leads to depression. Some of the most common environmental and social triggers include:
Depression can affect anyone, at any age, but certain factors can increase your risk. Statistically, depression often begins in the teens, 20s, or 30s. Rates of depression are higher in women, though this might be partly because women are more likely to seek treatment. A family history of depression, bipolar disorder, or alcoholism is a major risk factor.
Having other mental health conditions, like an anxiety disorder or post-traumatic stress disorder, also raises your risk. Similarly, people with serious or chronic illnesses such as cancer, stroke, or chronic pain are more likely to develop depression. Certain personality traits, like low self-esteem or being highly self-critical, can also make you more vulnerable.
Finally, older adults can be at risk, though depression is not a normal part of aging. Unfortunately, it often goes undiagnosed in this population. Being part of an unsupportive environment, especially for LGBTQ+ individuals, can also significantly increase the risk.
It can be difficult to watch a loved one struggle. Recognizing the signs of depression in others is the first step you can take to help them. The depressive symptoms they show might be subtle at first, but paying attention to changes in their mood and behavior can make a huge difference.
Your support might be what encourages them to seek mental health services. The symptoms of depression can look different depending on a person's age. Let's examine the warning signs in adults, children, and teenagers.
In adults, the signs of depression often align with the classic symptoms, such as sadness, loss of interest, and fatigue. However, in older adults, the presentation can be different and sometimes less obvious. Depression is not a normal part of advanced age, but it is often missed or mistaken for other health conditions.
For example, older adults may not talk about feeling sad. Instead, their depression might show up as physical aches or pain, memory difficulties, or personality changes. They may have a loss of appetite, sleep problems, or lose interest in sex. These symptoms can be mistakenly attributed to other medical issues or medications.
A key behavioral change to watch for in older adults is wanting to stay at home more often rather than socializing. Irritability and frustration can also be common signs. Key warning signs in this group include:
Depression in children and teenagers can be tricky to spot, as their symptoms may differ from adults. In younger children, depression might look like sadness, but it can also present as irritability, clinginess, worry, or refusing to go to school. They might also complain of aches and pains that have no clear physical cause.
As children become teenagers, their symptoms may evolve. Common signs in teenagers include sadness, irritability, and feeling negative or worthless. You might notice poor performance in school, anger, or feeling extremely sensitive and misunderstood. Behavioral changes are also a big clue.
A teen who once had a vibrant social life might suddenly withdraw from friends, use alcohol or drugs, or engage in self-harm. Recognizing this mood disorder early in young people is crucial for preventing more severe mental health disorders down the road. Common signs include:
If you think you or a loved one is struggling with depression, please know that help is available and you are not alone. Depression is one of the most treatable mental health conditions, with 80% to 90% of people responding well to treatment. The first step is reaching out. You can start by talking to a primary care provider, a mental health professional, or even a trusted friend or family member. If you are having thoughts of suicide, please call or text 988 to reach the Suicide & Crisis Lifeline immediately.
There are many effective treatment options, from talk therapy to medication. Your journey to mental health treatment is personal, and finding the right combination of support is key. The sooner you seek help from mental health services, the sooner you can start feeling better.
Getting a diagnosis of depression is the first step toward recovery. Health professionals will conduct a thorough evaluation of your symptoms, medical history, and mental health history. They may also order tests to rule out other medical conditions that could be causing your symptoms. This process helps them identify the specific type of depression and recommend the best course of action.
When it comes to treatment, you have options. Psychotherapy, or talk therapy, is a very common and effective approach. Cognitive behavioral therapy (CBT) is a particular type of therapy that helps you identify and change unhealthy thoughts and behaviors. For some, medication like antidepressants may also be recommended to help balance brain chemistry.
In Houston, TX, you can find support through various resources. The Substance Abuse and Mental Health Services Administration (SAMHSA) has a national helpline, and local organizations can connect you with care. Your primary care provider is also an excellent starting point for finding mental health services.
Recognizing depression in yourself and others is a crucial step towards understanding and addressing this complex condition. Throughout this blog, we've explored the nuances of depression, including its symptoms, types, and potential causes. Understanding these elements can empower you and those around you to seek help when needed. Remember, mental health is just as important as physical health, and taking that first step can lead to a brighter path ahead. If you or someone you know is struggling, don’t hesitate to reach out for support. For expert guidance, consider consulting with Riaz Counselling, where compassionate professionals are ready to help you navigate through tough times.
Health professionals perform a diagnosis of depression by conducting a comprehensive mental health evaluation. They use criteria from the Diagnostic and Statistical Manual (DSM) to determine if your symptoms meet the threshold for a depressive disorder. They will also review your medical history to rule out other causes before recommending mental health treatment.
For those seeking cognitive behavioral therapy in Houston, several highly-rated mental health services are available. These centers have mental health professionals skilled in treating depressive symptoms. Riaz Counselling is one of the top-rated counseling centers in the area, known for its expertise in CBT for both anxiety and depression.
Yes, finding the right specialist is key. Many mental health professionals in Houston offer cognitive behavioral therapy for both teens and adults dealing with depression and anxiety. Riaz Counselling has mental health professionals who specialize in CBT for both age groups, providing tailored support for each individual's unique needs.
If you're searching for clinics offering proven mental health treatment, look for those that use evidence-based methods. Cognitive behavioral therapy is one such treatment. Many clinics in the Houston area offer this service, and Riaz Counselling provides evidence-based treatments like CBT to help clients manage depression effectively.
While mild symptoms of depression may sometimes lessen over time, clinical depression, or major depressive disorder, typically does not go away on its own. Untreated, it can worsen and lead to more serious problems. Seeking professional help is essential for managing your mental health and achieving long-term recovery.
If you feel that you or someone you know, may benefit from therapy, please reach out to our office for a FREE 15 minute consultation: LINK
Stay informed about the latest research in psychology.
.png)
Explore how Internal Family Systems (IFS) therapy heals trauma and restores self-leadership.
.png)
Explore how Internal Family Systems (IFS) therapy heals trauma, anxiety, and inner conflict.
.png)
A practical guide to recognizing, preventing, and healing teacher burnout in Houston schools.