
Do you ever get the "winter blues" when the days get shorter? Many people feel a little down during the colder, darker months. But for some, this change triggers something more serious than a fleeting low mood. This condition, known as seasonal depression or seasonal affective disorder (SAD), is a type of mood disorder that can significantly impact your mental health. These recurring depressive episodes affect how you feel, think, and handle daily activities, bringing on symptoms like persistent sadness and low energy.
Seasonal affective disorder is more than just feeling sad about winter; it's a recognized form of depression with a clear seasonal pattern. The symptoms of depression are real and can be disruptive, typically appearing during the late fall and winter months when daylight is scarce.
What sets this condition apart is its predictability. Unlike other forms of depression that can occur at any time, SAD is tied directly to the changing seasons. Let's explore what defines this condition, how it differs from major depression, and how to spot recurring patterns in your own mood.
Seasonal affective disorder is a specific form of depression characterized by a recurring seasonal pattern. According to the National Institute of Mental Health, these depressive episodes happen around the same time each year, typically lasting for about four to five months.
While most people associate SAD with winter, there are two main types. Winter-pattern SAD starts in the late fall or early winter and subsides in the spring. A less common form, summer-pattern SAD, involves depressive episodes during the spring and summer months.
The fundamental signs of SAD include many symptoms of major depression. You might experience a persistent sad or anxious mood, feelings of hopelessness, loss of interest in hobbies, fatigue, and difficulty concentrating. For a diagnosis, these symptoms must occur seasonally for at least two consecutive years.
It might surprise you to learn that SAD is not technically considered a unique disorder. Instead, the official diagnostic manual classifies it as major depressive disorder "with a seasonal pattern." This means it's a subtype of major depression, not a completely separate condition among mental disorders.
The primary distinction is the timing and predictability of the episodes. While major depression can arise at any point, SAD is defined by its recurrent seasonal pattern. The symptoms of depression emerge during a specific season and then fully remit or are replaced by non-depressive periods during other times of the year.
To receive this diagnosis, a person must experience depressive episodes during a specific season for at least two years in a row. Additionally, these seasonal episodes must be more frequent than any non-seasonal depressive episodes they may have had throughout their life. This clear pattern is the key differentiator from other types of major depression.
How can you tell if your annual slump is just a case of the winter blues or something more? The key is to look for consistent patterns in your mood changes. Paying attention to when your depressive symptoms start and end each year can provide important clues.
A diagnosis requires that these mood shifts occur during a specific time of year for at least two consecutive years. For most, this means symptoms appear in the late fall or early winter and disappear by the time early summer arrives.
Consider if you notice the following patterns:
Researchers are still exploring the exact causes of seasonal depression, but most evidence points to a key trigger: less sunlight. The reduction in daylight hours during fall and winter appears to set off a chain reaction in your body that can lead to depression.
This reaction involves a few critical components, including your internal body clock, or circadian rhythm, and changes in your brain chemistry. Key players like serotonin and melatonin, along with your vitamin D levels, are all affected. Let's look at how sunlight, hormones, and brain chemicals work together to influence your mood.
Your body runs on an internal 24-hour clock known as the circadian rhythm, which regulates your sleep-wake cycle, hormones, and mood. This internal clock is heavily influenced by sunlight. When you are exposed to light, it signals to your brain that it's time to be awake and alert.
During the winter months, the decrease in natural sunlight can disrupt your circadian rhythm. With less daylight, your body clock can shift and fall out of sync with your daily schedule. This disruption can make it difficult for your body to adjust to the shorter days and longer nights.
This internal confusion can directly lead to depressive symptoms. Your sleep patterns may be thrown off, causing you to oversleep and still feel tired. This lack of restorative sleep, combined with a misaligned body clock, contributes to the fatigue and low mood characteristic of seasonal depression.
Your brain chemistry plays a huge role in your mood, and two key chemicals are at the center of seasonal depression: serotonin and melatonin. Serotonin is a neurotransmitter that contributes to feelings of happiness and well-being. Research suggests that sunlight helps your brain maintain normal serotonin levels.
For people with SAD, reduced sunlight in the winter can cause serotonin levels to drop, leading to depressive symptoms. This effect may be worsened by a vitamin D deficiency, as vitamin D is believed to promote serotonin activity. Since your body produces vitamin D when exposed to sunlight, less sun means lower vitamin D and, in turn, less serotonin activity.
Meanwhile, melatonin, a hormone that regulates sleep, is also affected. The darkness of winter can trigger an overproduction of melatonin, leading to increased sleepiness and fatigue. These hormonal influences and changes in brain chemistry are powerful drivers behind seasonal mood shifts.
The simplest answer for why seasonal depression is more common in winter is the significant reduction in natural sunlight. Shorter daylight hours are the primary trigger that disrupts your body’s internal systems, setting the stage for mood disorders to emerge.
This lack of sunlight creates a domino effect. It throws your circadian rhythm off balance, which confuses your sleep-wake cycle. At the same time, it leads to lower levels of mood-boosting serotonin and vitamin D while increasing the production of sleep-inducing melatonin. This combination creates the ideal conditions for winter-pattern SAD to develop.
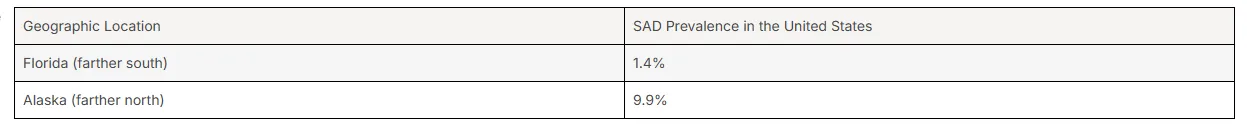
Geography provides further proof of this connection. The prevalence of SAD is much higher in people who live at northern latitudes, like in Alaska or New England, compared to those in sunnier states like Florida or Texas. The farther you are from the equator, the shorter the daylight hours are in winter, increasing your risk.
The signs of seasonal depression often mirror the symptoms of depression in general, but with some unique, season-specific additions. If you are experiencing SAD, you might notice significant changes in your mood and behavior during certain times of the year.
These depressive episodes can cause considerable emotional distress and disrupt your daily life. Common SAD symptoms include major shifts in sleep patterns, appetite changes that lead to weight gain, and a persistent feeling of sadness. It is important to remember that not everyone with SAD will have every symptom. Below, we'll explore the emotional, cognitive, and physical signs in more detail.
The emotional toll of seasonal depression can be heavy, affecting your thoughts and feelings in profound ways. This emotional distress goes far beyond simply feeling sad and can make it difficult to function as you normally would.
Many people experience a range of cognitive and emotional challenges. These can include:
It is crucial to take these symptoms seriously. In some cases, negative thoughts can escalate to include thoughts of death or suicidal thoughts. If you or someone you know is having these thoughts, it is vital to seek help immediately.
Seasonal depression doesn't just affect your mind; it has very real physical effects on your body and behaviors. These physical manifestations can drain your energy levels and interfere with your daily life, making even simple tasks feel overwhelming.
For winter-pattern SAD, which is the most common form, specific physical symptoms and behaviors often emerge. These can include:
In contrast, the rarer summer-pattern SAD can present with different physical symptoms, such as trouble sleeping (insomnia), poor appetite, and weight loss. These changes highlight how the condition can physically impact you in different ways depending on the season.
While seasonal depression most often begins in young adulthood, typically between the ages of 18 and 30, it can affect people of all ages. The way depressive symptoms present can vary depending on whether they appear in children, teenagers, or older adults.
Yes, children and teenagers can absolutely be affected. In younger individuals, SAD might manifest as irritability, sluggishness, and social withdrawal. Studies have also found a significant association between SAD symptoms and attention-deficit/hyperactivity disorder (ADHD), suggesting that young people with ADHD may be particularly vulnerable.
In older adults, symptoms might be linked to factors like a vitamin D deficiency, which is associated with low mood and worse cognitive performance. Regardless of age, if you notice a seasonal pattern of low energy levels and depressive symptoms in yourself or a loved one, consulting a mental health professional is a crucial step toward getting the right support.
Certain factors can make you more likely to develop seasonal depression. Demographics play a role, as the condition is diagnosed more often in women and tends to begin in young adulthood. Where you live is also a major risk factor.
Beyond these basics, your personal and family history can increase your vulnerability. Understanding these risk factors can help you recognize if you or a loved one belongs to one of the more vulnerable populations. Let's examine the specific demographic, geographic, and historical factors that put some people at a higher risk.
Demographically, SAD is diagnosed much more often in women than in men and typically starts when people are between 18 and 30 years old. However, one of the most significant risk factors is geography.
Your location in the United States and its proximity to the equator directly impacts your risk. People living in regions far north of the equator have a higher prevalence of SAD because they experience less daylight during the winter months. This is why someone in New England is more likely to have SAD than someone in Houston, TX.
The difference can be quite dramatic. Research shows a clear trend related to latitude, highlighting how crucial sunlight is for many people's mental health.
Your personal history with other mental health conditions is a significant predictor of your risk for seasonal depression. If you have already been diagnosed with major depression or bipolar disorder, you have a higher chance of developing a seasonal pattern to your symptoms.
The link is particularly strong for those with bipolar II disorder. Additionally, people with SAD often have other co-occurring mental health conditions, such as an anxiety disorder, an eating disorder, or panic disorder. A personal history of these issues can make you more vulnerable.
Family history also plays a part. SAD sometimes runs in families, so having a relative with the condition may increase your risk. Furthermore, if your family has a history of other mental illnesses, such as major depression or schizophrenia, you may also be more susceptible to developing seasonal affective disorder.
Although SAD typically emerges in young adults, it is important to recognize that it can also affect other vulnerable populations, including children and teenagers. The symptoms in younger people might look a little different, often presenting as increased irritability, fatigue, and withdrawal from social activities.
One study found that adults with ADHD were about three times more likely to have SAD symptoms, suggesting that children and teenagers with ADHD may be particularly at risk. Paying attention to seasonal mood changes in young people is essential for early identification and support.
Other vulnerable populations include older adults and anyone with pre-existing mental health conditions. In older adults, symptoms like low mood and cognitive decline have been linked to vitamin D deficiency, a key factor in winter-pattern SAD. This underscores the need to be aware of seasonal symptoms across the entire lifespan.
If you suspect you have seasonal affective disorder, it's important not to self-diagnose. The best course of action is to speak with a healthcare provider or a mental health specialist for a thorough evaluation and an accurate diagnosis. They can help rule out other conditions that might be causing your symptoms of depression.
The diagnostic process in clinical practice involves identifying a clear pattern of symptoms over time. If you are struggling, remember that help is available. For immediate support in a crisis, you can always call or text the 988 Suicide & Crisis Lifeline.
It is completely normal to feel a little down or have the "winter blues" from time to time. You might feel stuck inside more often, and the early darkness can be a drag. However, SAD is much more than an occasional low mood.
The key difference is that SAD is a form of major depressive disorder. Its sad symptoms are more severe, persistent, and disruptive to your daily life. Unlike the "holiday blues," which are tied to specific stressors, the depressive symptoms of SAD are linked to the time of year and the change in daylight.
To determine if your low mood is actually seasonal depression, a mental health professional will look for a specific pattern. The diagnosis requires that you experience these depressive episodes during a particular season for at least two consecutive years, with periods of remission in between. This recurring pattern is what separates SAD from a temporary dip in your mental health.
When you visit a healthcare provider, they may use certain screening tools, like a questionnaire, to help determine if your symptoms meet the criteria for SAD. This is part of a comprehensive evaluation to understand what you're experiencing.
So, when should you seek professional help? The time to reach out to a mental health professional is when your symptoms of depression start to interfere with your daily life. If you notice significant changes in your mood, thoughts, and behavior that recur with the seasons, it is a good idea to seek mental health services.
Consider seeking help if you experience any of the following:
In clinical practice, a diagnosis of seasonal depression is made after a comprehensive evaluation by a qualified mental health professional. There is no blood test or scan; instead, the diagnosis is based on your reported symptoms and their specific pattern over time.
According to the American Psychiatric Association, SAD is not listed as a standalone disorder in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). Instead, it is diagnosed as a "specifier" for major depressive disorder, officially called "Major Depressive Disorder with Seasonal Pattern."
To meet the criteria for this specifier, a person must show a clear temporal relationship between the onset of their symptoms of seasonal affective disorder and a particular time of the year. The pattern must have occurred for at least two years, with seasonal depressive episodes outnumbering any non-seasonal ones.
The good news is that there are several effective treatment options and management strategies available for seasonal depression. You don't have to simply endure the symptoms until the season changes. Help is available to get you feeling like yourself again.
Treatments fall into four main categories: light therapy, psychotherapy (like cognitive behavioral therapy), antidepressant medications, and vitamin D supplements. These approaches can be used alone or in combination to create a personalized plan that works for you. Let's explore some of these effective options in more detail.
Since the 1980s, light therapy has been a primary treatment for winter-pattern SAD. The goal is to compensate for the lack of natural sunlight by exposing you to bright light from a special light box. These boxes emit 10,000 lux of light, which is about 20 times brighter than typical indoor lighting.
To use a light box, you typically sit in front of it for about 30-45 minutes each morning. You don't stare directly at the light; instead, you keep it nearby while you read, eat, or work. The light box filters out harmful UV rays, making it a safe option for most people.
Light therapy is highly effective for managing the symptoms of seasonal affective disorder. Here’s what to know about its benefits:
In addition to formal treatments, certain lifestyle modifications can make a big difference in managing your symptoms and improving your daily life. Small, consistent changes can boost your mood and energy levels throughout the challenging months.
Are you wondering what you can do at home? Here are some lifestyle changes that can help:
Because SAD is so predictable, you can also take preventative measures. Starting treatments or lifestyle modifications in the fall, before symptoms even begin, can help reduce their severity or even prevent an episode altogether.
Understanding seasonal depression is crucial, as it affects many individuals at different stages of life. By recognizing its signs and symptoms, the underlying causes, and effective treatment options, you can take proactive steps towards managing this condition. Seasonal Affective Disorder (SAD) can significantly impact your quality of life, but with the right strategies in place, you can mitigate its effects. Remember that reaching out for help is a vital part of the process; whether through light therapy, lifestyle changes, or professional support, there are numerous avenues to explore for relief. If you're seeking guidance on managing seasonal depression, consider connecting with Riaz Counseling, where expert assistance is just a step away.
Seasonal affective disorder (SAD) is a form of depression that occurs in a recurring pattern with the changing seasons. The symptoms of seasonal affective disorder, such as low mood and fatigue, most often appear during the winter months. If you suspect you have SAD, it is best to consult a mental health professional for an accurate diagnosis.
Seasonal depression is primarily caused by a lack of sunlight during the shorter days of fall and winter. This reduction in sun exposure disrupts the body's internal clock (circadian rhythm) and can lead to lower levels of mood-regulating chemicals like serotonin and vitamin D, contributing to the "winter blues" and more severe symptoms.
Yes, talk therapy is a highly effective treatment. Cognitive behavioral therapy (CBT) in particular has been adapted for SAD and helps people challenge and change negative thoughts and behaviors associated with the season. It has been shown to produce some of the longest-lasting improvements for symptoms of depression and overall mental health.
For expert support in managing seasonal affective disorder in Houston, you can find a qualified mental health professional at Riaz Counseling. Seeking professional mental health services is a key step toward feeling better. For immediate help in a crisis anywhere in the United States, call or text the 988 Suicide & Crisis Lifeline.
In Houston, several top-rated counseling centers provide cognitive behavioral therapy for anxiety. Riaz Counseling is highly recommended, alongside others like The Houston Center for Cognitive Behavioral Therapy and The Anxiety Treatment Center. Each center specializes in tailored treatment plans to address individual needs effectively.
If you feel that you or someone you know, may benefit from therapy, please reach out to our office for a FREE 15 minute consultation: LINK
Stay informed about the latest research in psychology.
.png)
Explore how Internal Family Systems (IFS) therapy heals trauma and restores self-leadership.
.png)
Explore how Internal Family Systems (IFS) therapy heals trauma, anxiety, and inner conflict.
.png)
A practical guide to recognizing, preventing, and healing teacher burnout in Houston schools.