
Here are the key takeaways about gender differences and mental health:
Have you ever wondered if men and women experience mental health differently? The answer is a resounding yes. While mental health problems can affect anyone, there are clear gender differences in the types of conditions people face and how they seek help. A systematic review of current data shows that factors from biology to social roles play a part. Understanding these variations is crucial for public health and for improving mental health outcomes for everyone, ensuring care is both effective and accessible.
In a diverse city like Houston, understanding the nuances of mental health is key. Throughout the United States, gender differences significantly shape who seeks mental health care and what kind of support they receive. These patterns are reflected in communities across Texas, influencing everything from diagnosis to treatment.
Exploring these gender-based trends helps us see why mental health services must be tailored to meet diverse needs. How does gender affect the prevalence of mental health disorders in your community? Recognizing these differences is the first step toward better mental health outcomes for all residents. Now, let's look closer at how gender is defined and the role it plays in mental wellness.
When we talk about gender and mental health, it's important to distinguish between sex and gender. "Sex differences" refer to biological factors, like hormones, while "gender" relates to the socially constructed roles, behaviors, and expectations placed on men and women. These gender roles can create a "double standard" for mental wellness.
A classic 1970 study revealed this bias. Mental health professionals described a healthy adult and a healthy man with words like "independent" and "decisive." However, they described a healthy woman as "passive" and "emotional"—traits otherwise linked to being unhealthy. This shows how stereotypes can shape our very definition of what it means to be mentally well.
This double standard has real consequences. It influences how mental health problems are perceived, diagnosed, and treated. The main differences in mental health issues between men and women often fall along these stereotypical lines, with women experiencing more internalizing disorders and men more externalizing ones.
So, why is it important to study gender differences in mental health today? Current research shows us that these disparities have a massive impact on public health. For instance, major depression is a leading cause of disability for women worldwide, highlighting a critical need for targeted support.
Understanding these differences helps us move beyond a one-size-fits-all approach to mental healthcare. It allows for the development of more effective prevention strategies and treatments that acknowledge the unique pressures and biological factors affecting different genders. Ignoring these variations means we might be missing the mark in helping people effectively.
Studying these differences is crucial for:
American society plays a significant role in shaping gender-based mental health differences. Cultural norms in the United States often dictate how men and women are expected to express emotions and handle stress. For example, traditional masculinity can discourage men from admitting vulnerability or seeking help for mental health conditions.
This reluctance can lead to under-diagnosis and a reliance on potentially harmful coping mechanisms. In contrast, women are often more encouraged to discuss their feelings, which may contribute to higher rates of diagnoses for certain conditions and greater use of mental health services.
These societal pressures influence who walks through the door of a therapist's office and what symptoms they report. The way American culture defines strength and weakness along gender lines directly impacts how individuals manage their mental wellbeing, creating distinct patterns of mental health challenges.
While the overall prevalence of mental health disorders is nearly identical for men and women, the types of disorders diagnosed show clear gender patterns. Women experience significantly higher rates of internalizing disorders, such as major depression and anxiety. This disparity is one of the most consistent findings in mental health research.
For example, women are more than twice as likely as men to report a major depressive episode and nearly twice as likely to have an anxiety diagnosis. These depressive symptoms not only affect more women but also tend to persist longer. Let's examine the common disorders found among women and men more closely.
Women are more frequently diagnosed with what are known as "internalizing" disorders, where psychological distress is turned inward. Depressive disorders are at the top of the list, with women being diagnosed with major depressive disorder at more than double the rate of men.
Anxiety disorders are also notably more common among women. This category includes conditions like panic disorder, generalized anxiety disorder, and phobias. The impact of these conditions is often more severe for women, creating a greater burden on their daily lives. Physical and sexual violence, which disproportionately affects women, is considered a major contributing factor to these higher rates.
Some of the most common mental health disorders among women include:
Yes, certain mental health disorders are more common in men, and they typically fall under the "externalizing" category. These are conditions where distress is expressed through outward behaviors. Substance abuse is a primary example, with men having nearly three times the rate of alcohol abuse compared to women.
Men are also more likely to engage in binge drinking and use illicit drugs. This pattern is often linked to societal pressures on men to manage stress without showing emotional vulnerability. Additionally, men are more frequently diagnosed with neurodevelopmental disorders like autism and ADHD in childhood.
While women attempt suicide more often, men have a much higher rate of death by suicide. This tragic outcome is often linked to undiagnosed mental disorders, like depression or substance abuse, combined with lethal means. Common disorders in men include:
While many mental health conditions show a gender divide, some are shared more equally. Certain mood disorders and anxiety-related issues affect both men and women, although the expression of symptoms might still differ.
For instance, social anxiety disorder and obsessive-compulsive disorder (OCD) are found at roughly equal rates in both genders. Schizophrenia and borderline personality disorder also affect men and women with similar prevalence, though the age of onset and severity can vary. For example, schizophrenia symptoms often appear earlier in men.
Even with shared conditions, gender can play a role. Major depression, while more common in women, is still a significant issue for men, though it may present as anger or irritability rather than sadness. Mental health problems common to both genders include:
Did you know that gender differences in mental health don't just appear in adulthood? Mental health research shows that half of all mental health conditions begin by age 14. During childhood and early adolescence, we start to see distinct patterns emerge between boys and girls.
These early years are critical. The variations that start in childhood often become more pronounced as young people move through puberty and into early adulthood. For adolescent girls, especially, this period can mark the beginning of higher rates of depression and anxiety. Let's explore how these differences show up in youth and the impact of puberty.
During childhood, gender differences in mental health are already apparent. Boys are more frequently affected by neurodevelopmental conditions like autism spectrum disorder and ADHD. They are also about three times more likely than girls to be diagnosed with conduct disorders.
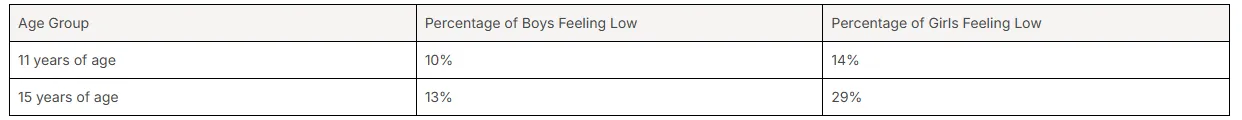
As young people enter adolescence, the picture shifts. This is when we see a significant rise in internalizing disorders, particularly among adolescent girls. For example, at age 11, 14% of girls report "feeling low" more than once a week compared to 10% of boys. By age 15, this gap widens dramatically: 29% of girls feel low compared to just 13% of boys.
This period marks a crucial divergence. While boys continue to show higher rates of externalizing issues, girls begin to experience the mental distress, anxiety, and depressive symptoms that will become more prevalent for women in adulthood. Understanding these early trends is key to providing timely support.
Puberty is a major turning point for mental health and heavily influences the gender differences we see. The hormonal changes that occur during this time interact with social and environmental pressures, creating a perfect storm for the emergence of certain mental health challenges. These biological sex differences contribute directly to the varying experiences of boys and girls.
For girls, the onset of puberty is strongly linked to a higher prevalence of depressive symptoms and anxiety. The flood of hormones like estrogen, combined with increasing societal pressures related to appearance and social roles, can trigger internalizing disorders. This is a key reason why the gender gap in depression opens up during the teenage years.
For boys, the hormonal shifts of puberty can be associated with different challenges, such as increased risk-taking behaviors. While the link isn't as direct as with depression in girls, puberty is a period where both biological and social factors begin to solidify the distinct mental health pathways for each gender.
Age trends reveal that gender differences in mental health diverge most sharply during adolescence. While some differences exist in early childhood, the years of age between 11 and 15 are a critical period of divergence. Life events and hormonal changes during this time amplify these variations.
Before this period, some disorders like ADHD are more common in boys. However, as teens navigate puberty, the prevalence of internalizing disorders skyrockets for girls. This divergence continues throughout the life course, establishing the patterns seen in adulthood, where women have higher rates of depression and anxiety, and men have higher rates of substance use.
The table below illustrates this divergence using data on adolescents feeling "low."
Beyond social pressures, what biological factors explain the gender differences in mental health? Your biology plays a surprisingly large role. A combination of hormonal factors, genetic predispositions, and neurobiological differences contributes to why men and women may be more vulnerable to certain conditions.
These internal mechanisms interact with your environment, but they create distinct pathways for mental wellness. For instance, hormones can influence neurotransmitters that regulate mood, while genetics can pass down a risk for specific disorders. Let's take a closer look at how these biological elements shape mental health across genders.
Hormonal factors are a major driver of the sex differences seen in mental health. Hormones like estrogen and testosterone don't just shape physical development; they also interact with brain chemistry. In women, estrogen affects neurotransmitters like serotonin, which is closely linked to mood regulation.
Fluctuations in estrogen levels throughout a woman's life—during puberty, the menstrual cycle, and perimenopause—can contribute to a higher risk for depressive symptoms and major depression. For example, some studies suggest that estrogen may have a protective effect against schizophrenia, which could help explain some of the differences in how the disorder presents in men and women.
These hormonal influences help explain why:
Genetics also contribute to the mental health landscape, but the role of gender is complex. While genetic predispositions for a mental illness can be passed down to anyone, how those genes are expressed can sometimes differ between men and women. The risk might be the same, but the outcome could be different.
For instance, research is exploring whether certain genes linked to major depressive disorder have a more powerful effect in women, especially when combined with hormonal factors and life stress. The interplay between your genes and your environment is crucial, and gender can be the lens through which that interplay is focused.
So, are genetic factors different? It’s not that the genes themselves are different, but their interaction with biological sex and gendered life experiences can lead to different mental health outcomes. This area of research is still growing but points to a deeply interconnected system of risk.
The brain itself shows subtle neurobiological differences between genders that can affect mental wellbeing. These are not about one brain being "better" than another but about variations in structure, chemistry, and circuitry. For example, how the brain processes stress and emotion can differ.
Child abuse and trauma can create long-term changes in brain circuitry, increasing the risk of anxiety and mood disorders. Since girls experience higher rates of certain types of violence, their brains may be uniquely impacted, leading to higher rates of psychological distress later in life.
These neurobiological variations can influence everything from emotional regulation to cognitive function. They help explain why women might be more prone to internalizing disorders rooted in emotional processing, while men might exhibit different responses. Understanding these differences is key to developing targeted and effective treatments.
Beyond biology, the world around you plays a huge part in your mental health. Sociocultural factors, including cultural norms and traditional gender roles, create different pressures and expectations for men and women. These social factors can either protect your mental health or make you more vulnerable.
How does your culture teach you to handle stress, express emotion, or ask for help? The answers are often tied to gender. These unwritten rules influence everything from your risk of developing a disorder to your willingness to seek treatment. We'll now explore how gender roles and cultural norms specifically shape mental health.
Gender roles and their associated behavioral expectations are powerful forces in mental health. From a young age, many societies teach boys and girls to behave in specific ways. Girls may be socialized to internalize their feelings, while boys are often taught to "act out" or suppress emotional displays.
This early socialization sets the stage for how adults cope with stress. When faced with mental distress, women may be more likely to develop internalizing responses like depression and anxiety. In contrast, men might turn to externalizing behaviors such as substance abuse or engaging in antisocial acts.
Traditional gender roles for women, which can offer fewer choices and lower life satisfaction, are also linked to higher rates of mental health problems. The pressure to conform to these roles can be a significant source of chronic stress. Gender roles influence:
Within the United States, regional cultural norms can add another layer to how gender and mental health interact. In Texas, as in many parts of the country, ideals of stoicism and self-reliance can be particularly strong, especially for men. This can create a significant barrier to seeking mental health care.
Admitting to a mental health struggle might be perceived as a sign of weakness, conflicting with traditional masculine ideals. This cultural pressure can lead men to delay seeking help until their symptoms are severe, sometimes resulting in involuntary commitment rather than outpatient care.
For women, cultural norms may be different, but they still present challenges. While they may be more likely to seek help, they might also face judgment or dismissal of their symptoms. Understanding these local cultural attitudes is essential for creating mental health care systems that are truly accessible and effective for everyone in the community.
Your family structure and community are foundational to your mental health. A strong network of social support can be a powerful protective factor, but the nature of that support often differs by gender. How do family and community impact men and women differently?
For women, having a diverse range of social roles—such as being a partner, parent, employee, and friend—is linked to a stronger sense of identity and better mental health. Strong community ties and emotional support are crucial. Conversely, being in a position of low social standing or feeling isolated can increase the risk of depression and anxiety.
For men, family and community can also be a source of strength, but the expectation to be a provider can add immense pressure. A lack of close, confiding relationships can leave men feeling isolated even when surrounded by people. Family and community influence mental health by:
The patterns of gender and mental health we see in the U.S. are not universal. Looking at cross-national data from the World Health Organization and studies in European countries gives us a broader perspective on world mental health. These comparisons reveal how much cultural context matters.
Different societal attitudes toward gender, varying levels of access to healthcare, and economic conditions all contribute to different outcomes. Do gender gaps in mental health look the same everywhere? Let’s compare the situation in Houston and the U.S. with international findings to find out.
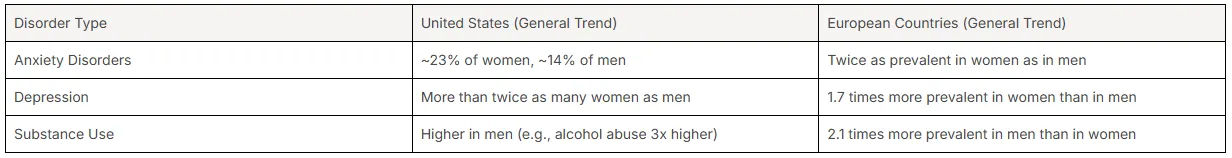
When comparing mental health outcomes in the United States with those in European countries, we see both similarities and differences. Data shows that in most places, women have higher rates of internalizing mental health disorders like anxiety and depression, while men have higher rates of substance use disorders.
However, the size of this gender gap can vary. In some western European countries, the prevalence of mental disorders in women is significantly higher than in men, and women are more likely to seek professional help. In some eastern European countries, the reported gap is smaller, which may be influenced by factors like stigma and access to care rather than a true difference in prevalence. Houston's outcomes reflect the broader trends seen across the United States.
Here is a general comparison of prevalence patterns:
Societal attitudes toward gender have a direct and measurable impact on mental health. Yes, research shows that a country's level of gender equality relates to mental health outcomes for both men and women. In social contexts where gender equality is higher, mental health tends to be better overall.
Studies using measures like the Global Gender Gap Index have found that in more gender-unequal countries, women's mental health is significantly worse. For example, low gender equality scores are associated with higher levels of depressive symptoms in women. The effects of this disadvantage can accumulate over a lifetime, leading to more pronounced health issues in older age.
Promoting gender equality is not just a matter of social justice; it's a public health imperative. Creating societies where opportunities and expectations are not limited by gender can foster better mental wellbeing for everyone, demonstrating how deeply social and personal health are intertwined.
Migration adds another layer of complexity to the relationship between gender, culture, and mental health. The process of acculturation—adapting to a new culture—can be a major source of stress, and its effects often differ by gender. How does this process affect mental wellbeing?
Immigrant women may face unique challenges, such as navigating new gender roles that conflict with their culture of origin, social isolation, and the stress of caring for a family in an unfamiliar environment. These cultural factors can increase their vulnerability to depression and anxiety.
For men, the pressure to find work and provide for their family in a new country, potentially with language barriers or discrimination, can be immense. The loss of social status they may have held in their home country can also impact their mental health. Acculturation effects include:
Mental health stigma is a powerful barrier to care, and it doesn't affect everyone in the same way. Gender stereotypes heavily influence how this stigma is experienced. The fear of being judged can prevent someone from seeking help for anything from social anxiety disorder to depression.
For men, the stigma is often tied to ideals of strength and stoicism, while for women, it can be linked to being overly emotional or dramatic. These stereotypes shape who feels comfortable admitting they are struggling. Let’s examine the specific ways that stigma impacts men, women, and nonbinary individuals.
Mental health stigma impacts men in a particularly challenging way. Cultural patterns of male stoicism and a reluctance to appear vulnerable create a powerful disincentive for men to admit they have a mental illness. Asking for help can feel like a failure to live up to masculine ideals.
As a result, men are more likely to ignore mental health problems in their early stages. They may not recognize their own depressive symptoms, which can manifest as anger or irritability rather than sadness. This reluctance to seek help is a major reason why men are underrepresented in mental health statistics, even when their symptoms are severe.
This stigma can lead to tragic consequences, as many men wait until a crisis point before getting support. The impact of stigma on men includes:
While women are generally more likely to seek help, they face their own unique forms of mental health stigma. Women who express symptoms of depressive disorders or anxiety may be dismissed as being "too emotional," "dramatic," or "hormonal." Their legitimate psychological distress can be trivialized.
This type of stigma can be incredibly invalidating and may lead to misdiagnosis. For example, a woman's physical symptoms caused by stress might be overlooked or not taken seriously by medical professionals. In cases of social anxiety, a woman might be labeled as just "shy" rather than being identified as needing support for a clinical condition.
Even though women seek help more often, the quality of that help can be compromised by gender stereotypes. The stigma they face is less about whether they should seek help and more about whether their struggles will be taken seriously once they do.
Nonbinary and transgender individuals face unique and compounded mental health challenges related to stigma. Unfortunately, research has historically excluded these populations, so there is limited data on prevalence and treatment. However, it is clear that they experience significant stressors.
These individuals often face stigma not just for their mental health conditions but also for their gender identity. This can come in the form of discrimination, rejection from family, and a lack of understanding from healthcare providers. This constant stress significantly increases the risk for anxiety, depression, and suicidal ideation.
Finding affirming social support and competent healthcare is a major challenge. The unique mental health hurdles for nonbinary and transgender people include:
When you look at mental health statistics, a clear gender gap emerges. It’s not that one gender has more mental health issues overall, but the data shows a higher prevalence of certain disorders in women and others in men. So, what factors contribute to this statistical divide?
A systematic review of the data points to a mix of reporting bias, diagnostic criteria, and true differences in experience. Men’s reluctance to report symptoms and professionals' biases can skew the numbers, making it seem like women have more problems when that may not be the whole story. Let's dig into the reasons behind these statistical gaps.
Several key reasons explain the gender-based differences we see in mental health statistics. One of the biggest is under-reporting by men. Due to social pressures, men are less likely to admit to or seek help for their symptoms, so they don't get counted in the data.
Diagnostic criteria and clinical bias also play a role. The very definitions of some disorders may better align with how women typically express distress. For instance, clinicians are more likely to diagnose women with depression than men, even when they present with identical symptoms, indicating a persistent gender bias in assessment.
Finally, there are genuine differences in risk factors. Women have higher exposure to certain traumas like sexual assault, which is a major driver of anxiety and PTSD. The reasons for the statistical gap include:
Collecting accurate mental health data by gender is filled with challenges. The primary obstacle is that most data relies on self-reporting or diagnoses from healthcare services. If a group is less likely to report symptoms or seek care, they will be underrepresented.
This is a major issue in mental health research concerning men. Their tendency to avoid seeking help means that data collection often misses a large portion of the population that is struggling. This leads to an incomplete picture of men's mental health.
Furthermore, much of the existing research operates on a gender binary, excluding nonbinary and transgender individuals entirely. This gap in data collection means we know very little about the prevalence, prevention, or treatment needs of these populations, making it difficult to design inclusive mental health programs.
Under-reporting of mental health issues is not just a gender issue; it's prevalent in many diverse populations. A systematic review of studies shows that cultural beliefs, stigma, and lack of access to culturally competent mental health care are major causes.
In some cultures, mental illness is seen as a family shame or a personal weakness, which strongly discourages individuals from speaking up. Language barriers and a mistrust of the healthcare system, often rooted in historical inequities, can also prevent people from seeking or reporting their struggles.
This under-reporting means that the true prevalence of mental health conditions in diverse communities is likely much higher than official statistics suggest. Key causes of under-reporting include:
Depression and anxiety are two of the most common mental health challenges, but they don't look the same for everyone. When we look at major depressive disorder and conditions like social anxiety disorder, clear gendered patterns emerge. The key differences often lie in prevalence and symptom expression.
Women are diagnosed with depression and most anxiety disorders at much higher rates than men. However, both genders can suffer deeply from these conditions. Understanding these patterns is critical for providing effective mental health care. Let's explore how depression and anxiety manifest in women and girls versus men and boys.
For women and girls, depression and anxiety often manifest as internalizing symptoms. This means feelings of sadness, worry, and worthlessness are turned inward. Mental health research consistently shows that depressive symptoms become much more common in adolescent girls after puberty.
This pattern continues into adulthood, where women are more than twice as likely to be diagnosed with depression. Anxiety, including social anxiety and panic disorders, also has a higher prevalence among women. This is often linked to a combination of biological factors, hormonal fluctuations, and greater exposure to interpersonal stress and trauma.
Common depression and anxiety patterns in women and girls include:
How do depression and anxiety appear in men and boys? Often, they look very different than they do in women. Instead of sadness, depression in men may present as anger, irritability, or aggression. They might also engage in reckless behavior or turn to substances to cope.
Similarly, anxiety disorders in men might not always look like classic worry. It could manifest as a need for control, physical symptoms like headaches or stomach problems, or compulsive disorder behaviors. Because these symptoms don't fit the stereotypical picture of depression or anxiety, they are often misdiagnosed or missed entirely.
This externalizing expression of internal pain is a key reason why men's mental health struggles are frequently overlooked. Common patterns in men and boys include:
Coping strategies for mood disorders like anxiety and depression often differ significantly by gender, leading to different mental health outcomes. Women are generally more likely to employ emotion-focused coping strategies. This includes seeking social support, talking about their feelings, and trying to understand the source of their distress.
While this can be a healthy approach, it can sometimes lead to rumination, where a person gets stuck overthinking negative feelings, potentially worsening depression. However, the inclination to seek support is a major reason women are more likely to engage in therapy.
In contrast, men are more often socialized to use problem-focused or avoidant coping strategies. They might try to distract themselves with activities, work longer hours, or use alcohol or drugs to numb their feelings. This avoidance can prevent them from addressing the root cause of their distress and often makes the problem worse over time.
When it comes to substance use disorders (SUDs), there is a clear gender difference. Are SUDs more common in men or women? The data shows that men have significantly higher rates of alcohol abuse and illicit drug use, making this a major public health issue for them.
However, women are not immune, and the reasons they use substances can be different. The associated risk factors and pathways to addiction vary between genders. Let’s examine the prevalence rates, risk factors, and treatment barriers related to substance use for both men and women.
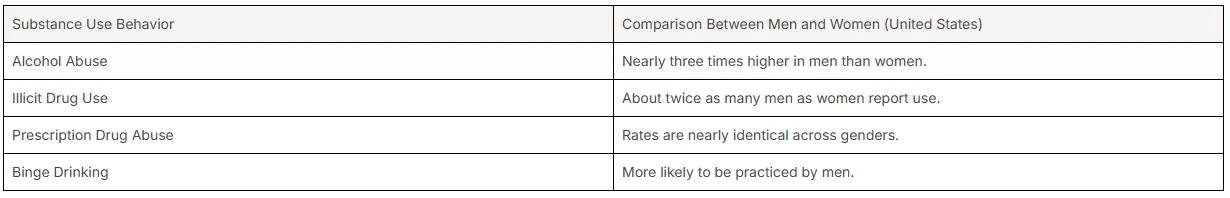
Across the United States, including in Texas, men are more likely than women to develop a substance use disorder. National data shows that men are more prone to engage in binge drinking and are nearly three times more likely to have an alcohol abuse disorder.
Men also report higher rates of illicit drug use. While specific data for Texas follows these national trends, the core patterns remain consistent. Men tend to use substances for thrill-seeking and pleasure, whereas women are more likely to use them to self-medicate for issues like trauma or abuse.
Interestingly, the rates of prescription drug abuse are nearly identical across genders, showing a different pattern of substance use. The table below highlights key gender differences in the United States.
The risk factors that drive substance use differ significantly by gender. For men, social factors related to masculinity often play a major role. The pressure to appear tough and in control can lead them to use alcohol or drugs to manage stress instead of seeking healthier outlets.
Thrill-seeking and peer pressure are also more prominent risk factors for men, particularly in their younger years. For many, alcohol use is normalized as a part of socializing and male bonding, which can escalate into dependency over time.
For women, the pathways to substance use are often different. They are more likely to start using substances to cope with the effects of trauma, abuse, or a co-occurring mental health disorder like depression. The goal is often self-medication rather than recreation. Key risk factors include:
Although men have higher rates of substance use, women are more likely to seek treatment. However, both genders face significant barriers to effective mental health care, and treatment outcomes can vary. A major barrier for men is the stigma around asking for help.
For women, barriers can be more practical. They may face difficulties with childcare, fear of losing their children, or financial dependence, all of which can prevent them from entering or completing a treatment program. This is a critical public health issue that the health care system needs to address.
To be effective, treatment programs must be gender-responsive. They need to address the different reasons men and women use substances, their unique triggers for relapse, and the specific social and economic barriers they face. A one-size-fits-all approach is often insufficient for achieving long-term recovery.
Experiences of trauma and abuse can have a devastating impact on mental health, and this impact is often gendered. How does trauma influence mental health differently by gender? The type of trauma experienced and the societal response to it can lead to very different mental health outcomes for men and women.
For example, women experience sexual abuse at much higher rates, which is strongly linked to conditions like PTSD, depression, and anxiety. The severity and duration of exposure to violence are directly correlated with being diagnosed with a mental illness. Let's explore these gender-specific impacts more deeply.
Yes, the rates of certain traumatic events and their mental health impact are starkly different by gender. Girls and women experience sexual abuse and assault at significantly higher rates than boys and men. According to the CDC, about one in four women suffer sexual assault or rape in their lifetimes.
This type of trauma has a profound and lasting effect on mental health outcomes. There is a particularly strong connection between sexual abuse and the development of posttraumatic stress disorder (PTSD). Women who were exposed to childhood violence have depression rates three to four times higher than those who were not.
While men also experience trauma, the types of traumatic events they face may be different (e.g., combat, physical assaults). The mental health consequences are just as real, but the specific pathways differ. Key points on impact include:
Domestic violence is a pervasive issue that causes immense psychological distress, and its mental health effects are deeply felt across genders. While both men and women can be victims, women experience it at higher rates and often with greater severity, leading to distinct mental health outcomes.
Victims of domestic violence are at a much higher risk for developing a range of mental health problems. The chronic stress, fear, and powerlessness inherent in an abusive relationship can trigger depressive symptoms, anxiety, PTSD, and substance use issues as a way to cope.
For women, the experience can be compounded by social and economic factors that make it difficult to leave, trapping them in a cycle of abuse that continually harms their mental wellbeing. For men who are victims, the stigma can be even greater, making it incredibly difficult to seek help or be believed.
Recovery from trauma and abuse is possible, but the pathways often need to be tailored to an individual's gender and experiences. A cornerstone of healing for anyone is access to safe, trauma-informed mental health care. This means working with professionals who understand the impact of trauma.
For many women, finding strong social support is a critical part of recovery. Support groups with other survivors can reduce feelings of isolation and shame. Therapy focused on processing the trauma, such as Trauma-Focused CBT or EMDR, can be highly effective.
For men, recovery paths may need to first address the stigma around vulnerability. Peer support groups specifically for male survivors can create a safe space to share experiences without judgment. Effective recovery paths often include:
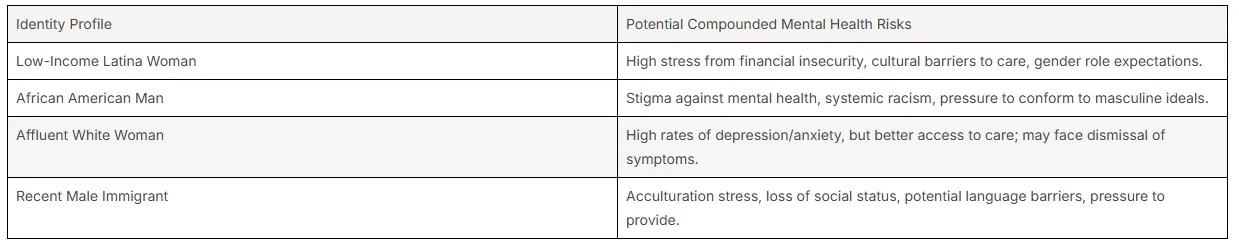
Your identity is not one-dimensional, and neither are your mental health risks. The concept of intersectionality helps us understand how different aspects of your identity—like gender, race, and socioeconomic status—overlap and interact. These intersecting factors can compound risk and create unique mental health outcomes.
For example, a woman of color living in poverty faces different challenges than a wealthy white man. Her experience is not just about being a woman, but about the combined effects of her gender, race, and economic situation. Let's look at how these intersections play out in a diverse city like Houston.
In a multicultural city like Houston, it's crucial to look beyond just gender. Ethnic and racial backgrounds, combined with socioeconomic factors, create varied mental health experiences. For example, some research indicates that the link between low gender equality and depressive symptoms is particularly strong for non-white women.
Different cultural groups may have varying levels of stigma around mental health, different expressions of distress, and unequal access to culturally competent care. A person's immigration status, language barriers, and experiences with discrimination all add layers of complexity to their mental wellbeing.
While the compiled data does not provide specific statistics for Houston's ethnic groups, we can illustrate the concept of intersectionality with a hypothetical table showing how risks can be compounded.
Access to mental health care frequently reflects underlying economic disparities, significantly impacting treatment outcomes. Individuals from lower socioeconomic backgrounds often face obstacles such as lack of insurance, transportation challenges, and fewer available services, which can exacerbate mental disorders like anxiety and depression. Research shows that women may experience these barriers more acutely, influenced by social factors like caregiving responsibilities. Meanwhile, men might turn to substance use as a coping mechanism. Addressing these gaps in access is essential for improving mental health outcomes, fostering gender equality and enhancing life satisfaction within our communities.
The interplay of various factors can significantly amplify the impact of mental health conditions. For instance, individuals experiencing substance abuse alongside anxiety disorders often face compounded challenges that exacerbate their mental health outcomes. This can lead to a cycle of mental distress that is difficult to break, particularly among vulnerable populations. Furthermore, social factors such as stigma, access to mental health services, and adverse life events can heighten these effects. Understanding these compound effects is crucial for addressing mental health disorders more effectively and tailoring interventions to meet the unique needs of diverse groups.
Tailored prevention and early intervention strategies acknowledge the distinct experiences faced by different genders regarding mental health. Programs designed for young people often focus on resilience-building and coping skills, which can address anxiety disorders and depressive symptoms specifically among adolescent girls and boys. For adults, gender-informed approaches may include community initiatives that prioritize social support systems, fostering healthy connections to alleviate feelings of isolation. Equally important is ensuring access to mental health services that consider biological and social factors, ultimately contributing to improved mental health outcomes across the lifespan.
Implementing school-based programs that address mental health can significantly improve outcomes for young people. These initiatives can reduce anxiety disorders, support mental well-being, and foster life satisfaction among students. By promoting awareness of mental health conditions, schools can create supportive environments that encourage open discussions about emotions and experiences. Moreover, focusing on youth within educational settings allows for early intervention and tailored approaches that align with the unique challenges faced during adolescence. Programs designed to bolster resilience and social support directly target risk factors associated with mental health problems and ultimately improve the overall mental health landscape for future generations.
Efforts in Texas to enhance community outreach and raise awareness about mental health demonstrate a commitment to addressing gender differences in mental health care. Local organizations are increasingly focusing on mental health education, ensuring that vulnerable populations, including adolescent girls and young adults, receive necessary support. By utilizing social support networks and engaging various community stakeholders, these initiatives aim to reduce stigma and promote understanding of mental health disorders. As a result, residents gain improved access to essential mental health services, leading to better mental health outcomes and overall quality of life for all, regardless of gender.
Recognizing the distinct mental health needs of adults, gender-informed approaches can enhance treatment effectiveness. Tailoring interventions to consider not just biological differences, but also social factors, has shown promise in improving mental health outcomes. For instance, addressing the higher prevalence of anxiety and depressive disorders among women through targeted support groups can foster better social connections and resilience. Moreover, understanding the impact of life events and cultural factors on mental health enables providers to address risk factors specific to each gender. By prioritizing these nuanced care models, we can improve overall life satisfaction and quality of life for adults experiencing mental health challenges.
Understanding individual experiences related to gender can lead to more effective mental health treatment. Tailoring approaches to everyone’s unique needs considers biological, psychological, and social factors that can influence mental health outcomes. For instance, women may face higher rates of mood disorders and depressive symptoms, while men might encounter more challenges with substance use disorders. Creating gender-specific strategies helps health care providers address these diverse risks and improve the quality of care. This personalized attention not only enhances life satisfaction but also fosters a supportive environment for mental health recovery among adults.
Addressing mental health concerns effectively requires recognizing the unique needs arising from gender differences. Personalized treatments must consider the specific risk factors associated with various genders, such as the distinct prevalence of anxiety disorders among young women and substance use disorders in men. Tailoring therapeutic approaches can enhance mental health outcomes, fostering a supportive environment that promotes recovery and resilience. By including gender-informed strategies and building social support networks, healthcare providers can improve life satisfaction for all individuals, paving the way for more equitable access to mental health services and better overall well-being.
Health providers in the U.S. play a critical role in addressing the complex landscape of gender and mental health differences. By understanding the unique risk factors and experiences that influence male and female mental health, they can tailor their approach to better meet individual needs. Health systems that prioritize gender-informed care not only improve treatment outcomes but also enhance patient satisfaction. By fostering environments that encourage open discussions about mental health, providers can help combat stigma and promote access to essential services. This collaborative approach is vital for improving overall mental health outcomes across diverse populations.
Identifying and addressing gaps in mental health services is essential for promoting equity among different genders. Advocating for equitable access to care involves not only recognizing the unique challenges faced by various groups but also implementing changes in public health policies. This can ensure that mental health resources are available to those most affected, such as young adults and those experiencing higher rates of mental health problems. By fostering an environment of social support, we can work towards reducing stigma and improving mental health outcomes for everyone, regardless of gender.
Understanding the intricacies of gender differences in mental health is vital for effective intervention and support. By recognizing how societal and biological factors contribute to disparities, we can develop tailored strategies that address specific needs. Whether through early intervention programs targeting young adults or adult-focused gender-informed approaches, creating a more equitable mental health landscape is essential. Engaging communities in awareness and education can empower individuals and enhance overall mental well-being, ultimately leading to improved life satisfaction and reduced mental disorders across varied demographics. Together, we can help pave the way for better mental health outcomes for all.
Gender differences in mental health issues often manifest through variations in prevalence, expression, and coping mechanisms. For instance, men may experience higher rates of substance abuse, while women are more likely to suffer from anxiety and depression. Tailored approaches are essential for effective treatment.
For those seeking a male or female therapist for anxiety in Houston, Texas, Riaz Counseling offers professional services tailored to individual needs. Their specialized team focuses on creating a supportive environment conducive to mental health recovery and personal growth.
Riaz Counseling in Houston is recognized for its effective use of Cognitive Behavioral Therapy (CBT) in managing anxiety. Their tailored approaches and experienced therapists have helped numerous clients overcome anxiety challenges, making them a reputable choice for those seeking support in this area.
Yes, mental health treatments are often tailored differently for men and women due to varying psychological responses, societal expectations, and biological factors. This personalized approach enhances effectiveness, addressing specific gender-related needs in mental health care. You can visit Riaz Counseling for more information.
Stigma surrounding mental health varies between genders, often manifesting as men facing pressure to appear strong and self-reliant, while women may experience judgment for expressing vulnerability. These differences can affect help-seeking behaviors and overall mental health outcomes.
If you feel that you or someone you know, may benefit from therapy, please reach out to our office for a FREE 15 minute consultation: LINK
Stay informed about the latest research in psychology.
.png)
Explore how Internal Family Systems (IFS) therapy heals trauma and restores self-leadership.
.png)
Explore how Internal Family Systems (IFS) therapy heals trauma, anxiety, and inner conflict.
.png)
A practical guide to recognizing, preventing, and healing teacher burnout in Houston schools.