
Here is a quick look at what we'll cover in this guide to tackling nurse burnout:
Nursing is a profession that demands immense physical and emotional strength. Healthcare workers are essential, but their dedication often leads to a serious challenge: nurse burnout. This isn't just a bad day at work; it's a recognized occupational phenomenon characterized by deep exhaustion. Understanding and addressing this issue is vital not only for the well-being of nurses but also for the health of the entire care system. Are you ready to explore what burnout is and how to fight it?
Nurse burnout is a critical public health issue that significantly affects healthcare delivery, not just globally but right here in communities like Houston, TX. When nurses face a high risk of burnout, the quality of patient care can decline, impacting everyone who relies on the medical system.
This widespread problem jeopardizes the stability of our healthcare workforce. To protect both nurses and patients, it is crucial to understand the specifics of burnout, how prevalent it is, and how it differs from the daily pressures of the job.
The World Health Organization (WHO) defines the burnout syndrome as an occupational phenomenon resulting from chronic, unmanaged workplace stress. It’s not simply feeling tired; it is a state of emotional, physical, and mental exhaustion that can feel all-consuming. Have you ever felt completely drained by your work? For many in nursing, this feeling is a daily reality.
This issue is not isolated to a few individuals. Nurse burnout has become a pervasive problem affecting healthcare professionals around the world, with some experts calling it an epidemic within the industry. The demanding nature of nursing, combined with systemic pressures, creates a perfect storm for this condition to develop and thrive.
Globally, a significant percentage of nurses report experiencing burnout symptoms. For instance, studies show that nearly 13% of new nurses feel burnt out within their first few years on the job. This highlights how widespread the issue is, impacting the nursing profession from the very beginning of a nurse's career.
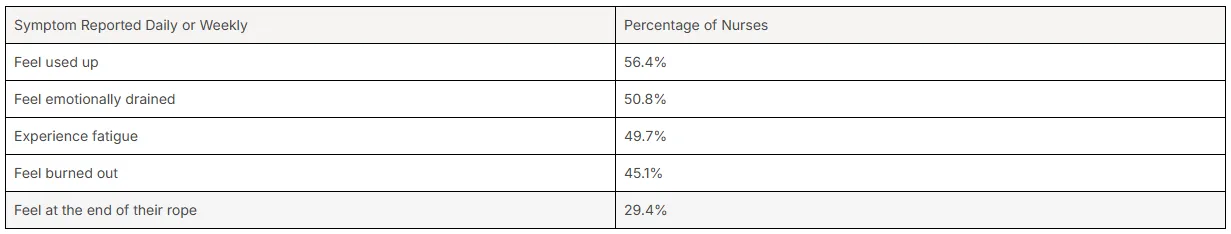
The risk of burnout within the U.S. healthcare system is alarmingly high. Recent data paints a stark picture of the emotional and physical toll on the nursing workforce. Research from the National Council of State Boards of Nursing (NCSBN) reveals just how many nurses are struggling.
This isn't a problem that can be ignored. The high prevalence of these feelings demonstrates an urgent need to address the root causes and provide better support for nurses. The data shows that a substantial portion of the nursing population feels exhausted and overwhelmed on a frequent basis.
A recent survey highlights the specific symptoms nurses report daily or weekly, emphasizing the severity of the issue across the nation.
Symptom Reported Daily or Weekly
It's important to distinguish between typical workplace stress and burnout, as they are not the same. Stress is often characterized by over-engagement, where you feel a sense of urgency and hyperactivity. Fatigue from stress is usually temporary and can be relieved with rest and a break from the stressful situation.
Burnout, on the other hand, is a state of profound emotional exhaustion and disengagement. Instead of hyperactivity, you feel helpless and detached. The exhaustion associated with burnout is not easily fixed with a long weekend; it’s a deeper, more persistent sense of being drained. It is a response to prolonged, overwhelming stress in your work environment.
Key burnout symptoms that set it apart from stress include cynicism, a sense of ineffectiveness, and emotional detachment from your work and patients. While stress can make you feel frantic, burnout makes you feel empty and apathetic, fundamentally changing your perspective on your job.

The causes of nurse burnout are complex and often rooted in the work environment itself. Factors like overwhelming professional responsibilities and systemic issues within health care contribute significantly to this growing problem. Do you feel like your workload is unmanageable? You are not alone.
From high patient loads to endless paperwork and the sheer emotional weight of the job, many elements combine to create a high-risk environment for burnout. Let's examine some of the main causes that push dedicated nurses to their limits.
One of the primary drivers of burnout is inadequate staffing, which leads to high patient-to-nurse ratios. When nurses are responsible for too many patients at once, they are stretched thin, making it nearly impossible to provide the level of direct patient care each person deserves. This constant pressure leads to increased stress and fatigue.
This overwhelming situation not only affects the nurse but also has a direct impact on patient outcomes. When a nurse's attention is divided among too many people, the risk to patient safety grows. The feelings of inadequacy and frustration that come from not being able to provide optimal care can be a heavy burden.
High patient-to-nurse ratios are associated with several negative consequences, including:
Beyond direct patient care, nurses are often swamped with a mountain of administrative tasks. Does it ever feel like you spend more time with paperwork than with patients? This is a common complaint and a significant contributor to burnout. Excessive documentation and other administrative duties take valuable time away from the hands-on care that drew many to the profession.
This shift in focus can lead to deep feelings of frustration and a lack of fulfillment. For many healthcare organizations, these administrative requirements are non-negotiable, yet they can negatively impact a nurse's job performance and morale. The core of nursing is caregiving, and when that is overshadowed by paperwork, job satisfaction plummets.
Ultimately, being burdened by these tasks prevents nurses from doing what they do best: caring for people. This disconnect between their passion and their daily duties is a powerful catalyst for burnout, making them question their role and their impact.
Nursing is an emotionally taxing profession. The constant exposure to suffering, pain, and loss takes a significant toll on a nurse's mental and emotional well-being. Providing compassionate care requires a deep level of empathy, but over time, this can lead to emotional exhaustion, a condition often called compassion fatigue.
This emotional strain is a key component of burnout. When nurses are constantly immersed in traumatic events and high-stakes situations, they may find it increasingly difficult to cope. This can lead to a state of decreased empathy and emotional numbness as a self-preservation mechanism.
Compassion fatigue makes it challenging for nurses to continue providing the empathetic, high-quality care patients need. The pressure to always be compassionate while dealing with personal emotional depletion is a heavy weight to carry and a direct path toward developing burnout over time.
How do you know if you are starting to experience burnout? Recognizing the early signs of nurse burnout is the first step toward preventing it from becoming overwhelming. These indicators can be both physical and emotional, signaling that your well-being is at risk.
Paying attention to these initial burnout symptoms allows you to take proactive measures before they escalate. From physical exhaustion to a change in your attitude toward work, let's explore the key warning signs that you should not ignore.
One of the most prominent signs of burnout is severe physical exhaustion. This isn't just feeling tired after a long shift; it's a persistent state of chronic fatigue that sleep doesn't seem to fix. Nurses often work long hours without adequate rest, leading to sleep deprivation and a feeling of being completely drained.
This exhaustion can make it difficult to perform even basic tasks, both at work and at home. When you're constantly running on empty, your ability to provide safe and effective care is compromised. This level of fatigue is often intertwined with emotional exhaustion, creating a cycle that is hard to break.
Are you experiencing any of these physical signs?
Another hallmark of burnout is a growing sense of emotional detachment from your job and your patients. This is often referred to as depersonalization, where you may start to view patients as tasks to be completed rather than as individuals needing care. This shift can lead to a lack of compassion that feels unnatural and distressing.
This detachment is often accompanied by cynicism. You might find yourself feeling increasingly negative or critical about your work, your colleagues, and the healthcare system as a whole. This cynicism can contribute to an unpleasant work environment, further fueling the cycle of burnout for you and those around you.
This emotional shift is a defense mechanism against overwhelming emotional demands, but it ultimately undermines the very essence of nursing. If you notice yourself becoming more cynical or disconnected, it's a clear sign that you need to address what's happening.
When burnout takes hold, your passion for nursing can begin to fade. A significant indicator is a noticeable decrease in job satisfaction and motivation. You may start to question your abilities or feel that your work no longer makes a meaningful difference. This can lead to feelings of professional inadequacy and frustration.
This loss of motivation isn't a personal failing; it's a natural response to a lack of support and overwhelming demands. For many nursing staff, feeling undervalued or like you are constantly falling short of expectations can erode the sense of accomplishment that once fueled your career.
Do you dread going to work? Do you feel like you are just going through the motions? This decreased motivation is a serious symptom of burnout that affects not only your well-being but also the energy you bring to your team and your patients.
The consequences of nurse burnout extend far beyond the individual nurse. This issue has a direct and serious impact on patient care, affecting everything from safety to satisfaction. When nurses are exhausted and disengaged, their ability to provide high-quality care is significantly compromised.
This decline in care quality affects the entire healthcare delivery system. How can patients receive the best care when their caregivers are struggling? Let's look closer at how burnout among nurses can lead to poorer outcomes and increased risks for patients.
There is a direct correlation between nurse burnout and negative patient outcomes. When nurses are burnt out, their cognitive abilities and attention to detail can suffer, which compromises patient safety. Studies have shown that hospitals with higher rates of nurse burnout tend to have higher rates of hospital-acquired infections and patient falls.
The quality of care is fundamentally linked to the well-being of the caregiver. An exhausted, emotionally detached nurse may struggle with critical decision-making and interpersonal interactions, which are essential for providing optimal care. This can lead to a general decline in the standard of care that patients receive.
Ultimately, burnout creates an environment where both nurses and patients are at risk. The inability to focus fully on patient needs can have serious consequences, turning preventable issues into significant health problems and undermining the core mission of healthcare.
One of the most dangerous consequences of nurse burnout is the increased risk of medical errors. Research has demonstrated a strong link between a nurse’s level of burnout and the likelihood of making a mistake, such as a medication error. Burnout impairs the crucial cognitive functions needed for safe practice.
The odds ratio for errors increases as symptoms of burnout, like emotional exhaustion, become more severe. Fatigued and overwhelmed nurses may miss critical details or shortcuts in procedures, which can have devastating results for patients. These aren't careless mistakes but rather symptoms of a strained and overloaded human system.
This reality poses a significant threat to health care systems everywhere. Preventing burnout is not just about supporting nurses; it is a critical patient safety initiative. By addressing the factors that lead to burnout, we can create a safer environment for everyone involved.
Burnout doesn't just affect one nurse in isolation; it can spread through a unit and poison team morale. A nurse experiencing cynicism and emotional detachment can contribute to a negative and unsupportive work environment. This negativity can impact collaboration among team members, making effective communication and teamwork more difficult.
When team morale is low, the entire unit's performance can suffer. A lack of camaraderie and trust hinders the seamless collaboration required in fast-paced medical settings. This can lead to breakdowns in communication, which may in turn compromise patient care and safety.
Fostering a supportive work environment is essential to counteract this effect. A positive organizational culture where nurses feel supported by their peers and leaders can buffer the effects of stress. However, when burnout is widespread, it systematically erodes the very foundations of a healthy and collaborative team.
While a heavy workload is a major cause of workplace stress, it's not the only factor driving nurse burnout. The work environment itself, including the level of autonomy and support a nurse receives, plays a huge role. Do you ever feel like you have no say in your own work?
Issues like a lack of control, an unsupportive culture, and limited access to emotional support can be just as damaging as long hours. These elements shape the day-to-day experience of healthcare delivery. Let's explore these other critical contributors to burnout.
A significant factor contributing to burnout is a lack of control and autonomy over one's work. Nurses often face rigid structures and a hierarchical environment where their ability to make decisions about their professional responsibilities is limited. This can lead to feelings of frustration and helplessness.
When nurses feel their expertise is undervalued or they lack the power to influence their work environment—for instance, through more flexible scheduling—it can erode their sense of professional worth. Being empowered to make decisions is a key component of job satisfaction.
Having more autonomy doesn't mean working without oversight; it means having a voice in shaping patient care processes and your own work life. Granting nurses more control can restore a sense of ownership and purpose, making them feel more like valued professionals and less like cogs in a machine.
An unsupportive organizational culture can be toxic for the nursing profession. When nurses feel isolated or unsupported by their colleagues and superiors, it becomes incredibly difficult to cope with the inherent demands of the job. A culture that lacks open communication and mutual respect is a breeding ground for burnout.
How does the culture at your workplace feel? A supportive culture is one where asking for help is encouraged, not seen as a weakness. It’s an environment where management actively listens to concerns and works to address them. Without this support, nurses are left to manage immense stress on their own.
Healthcare organizations have a responsibility to foster a culture that prioritizes the well-being of their staff. This includes everything from promoting teamwork to ensuring easy access to resources like employee assistance programs. A positive culture is one of the best defenses against burnout.
Even when nurses recognize they need help, they often face a significant barrier: limited access to mental health resources. The stigma surrounding mental health in the medical field, combined with a lack of available and affordable support, can prevent them from seeking the emotional support they desperately need.
Many large healthcare facilities offer Employee Assistance Programs (EAPs), which can provide free or low-cost therapy and referrals. However, not all organizations have these programs, and even when they do, nurses may not have the time or energy to use them. This gap in support is a critical public health concern.
Accessible mental health resources are not a luxury; they are a necessity for a healthy nursing workforce. Encouraging nurses to seek help and making that help readily available is a vital step in addressing burnout. This includes access to therapists, counselors, and support groups specifically tailored to the challenges of the healthcare profession.
The good news is that burnout is not inevitable. There are many effective strategies that can be used for burnout prevention. These approaches involve both individual coping strategies and broader organizational changes. Are you looking for ways to protect your own well-being?
From promoting a healthier work-life balance to encouraging peer support, these strategies empower nurses and create a more sustainable work environment. Let's look at some of the most effective ways to combat burnout and reclaim your passion for nursing.
One of the most crucial strategies for preventing burnout is promoting a healthy work-life balance. It is essential to establish clear boundaries between your professional responsibilities and your personal lives. Without this separation, the stress of work can easily spill over and dominate every aspect of your life, diminishing your overall quality of life.
Achieving this balance often requires conscious effort. This can mean learning to say no to extra shifts when you're already feeling stretched or making a point to disconnect completely from work-related communications during your time off. Organizations can support this by offering options like flexible scheduling.
To improve your work-life balance, consider these steps:
Developing personal coping strategies is a powerful way to manage the daily pressures of nursing. Mindfulness and other stress reduction techniques can help you stay grounded and calm your mind, even during a chaotic shift. The first step is often just taking a moment to breathe deeply and center yourself.
Practices like mindfulness meditation, progressive muscle relaxation, or even a short, mindful walk can significantly reduce stress levels. These techniques help you stay present and focused, preventing your mind from being overwhelmed by anxiety about the past or future. Have you ever tried a simple breathing exercise during a tough day?
Incorporating these practices into your daily routine can build resilience over time. Taking regular breaks throughout the day, even for just a few minutes, to rest and recharge is not a sign of weakness but a smart strategy for long-term well-being and effective caregiving.
You don't have to face the challenges of nursing alone. Building strong relationships with colleagues through peer support and mentoring can be a lifeline. Having trusted peers to talk to creates a safe space to share experiences and frustrations without judgment. This sense of camaraderie can combat the feelings of isolation that often accompany burnout.
Mentorship programs are particularly effective. Pairing experienced nurses with newer or struggling colleagues provides guidance, support, and encouragement. This not only helps with professional development opportunities but also fosters a culture of open communication and mutual respect within the team.
When nurses support each other, the entire work environment becomes healthier. Encouraging these connections helps build a resilient and collaborative team that can better navigate the stresses of the job together. A simple conversation with a colleague can make a world of difference.
While individual nurses can adopt coping strategies, true, lasting change must come from the top. Healthcare leaders and healthcare organizations have a critical role to play in burnout prevention. They have the power to create a supportive workplace culture that prioritizes the well-being of its staff.
What can hospital leaders do to make a real difference? From implementing better policies to leveraging technology, leaders can address the root causes of burnout systemically. Let's explore how leadership can transform the work environment for nurses.
The foundation of burnout prevention is a supportive workplace culture. Healthcare leaders must actively work to create an organizational culture where nurses feel valued, heard, and respected. This goes beyond just saying they support their staff; it requires concrete actions that build trust and boost team morale.
A supportive work environment is one where open communication is the norm, and feedback is encouraged and acted upon. Initiatives that increase nurse engagement, such as involving them in decision-making processes, can create a sense of ownership and increase job satisfaction. When nurses have a voice, they feel more empowered.
Leaders can build this culture by:
Meaningful policy changes are essential for systemic burnout prevention. Healthcare leaders and nursing associations are increasingly advocating for policies that directly address the most significant stressors in the healthcare system. One of the most critical areas is staffing.
Implementing safe nurse-to-patient ratios is a key policy change that can alleviate overwhelming workloads. Similarly, legislation that protects nurses from mandatory overtime ensures they have adequate time for rest and recovery. These changes promote a healthier work-life balance and reduce physical and emotional strain.
Collaboration between healthcare organizations, policymakers, and nursing professionals is vital to drive these changes forward. By working together to identify and reform the policies that contribute to burnout, the entire industry can create a more sustainable and supportive environment for the nursing profession.
Technology can be a powerful ally in the fight against burnout. By leveraging technology to improve workflow efficiency, healthcare organizations can reduce many of the burdens that contribute to nurse stress. For example, streamlined electronic health records (EHRs) can significantly cut down on the time nurses spend on administrative tasks.
When paperwork is reduced, nurses have more time to focus on what matters most: providing quality care and building meaningful connections with their patients. Additionally, smart alarm systems can help minimize unnecessary interruptions and chronic stress, allowing nurses to concentrate on critical needs without being constantly overwhelmed by non-urgent alerts.
Investing in the right technology is an investment in the well-being of the nursing staff. By automating and simplifying tasks, technology helps create a more efficient and less stressful work environment, ultimately supporting both nurses and the patients they care for.
In conclusion, addressing nurse burnout is crucial for both the wellbeing of healthcare professionals and the patients they serve. Understanding the multifaceted causes of burnout, from excessive workloads to insufficient support, is key to implementing effective strategies that promote a healthier work environment. By prioritizing work-life balance, encouraging mindfulness practices, and fostering peer support, nurses can begin to reclaim their passion for their profession. Additionally, healthcare leaders play a significant role in creating a supportive organizational culture that mitigates burnout risks. Remember, seeking help is vital. If you're in Houston and struggling with burnout, don't hesitate to reach out to Riaz Counseling for support tailored to your needs. Together, we can work towards a healthier future in nursing.
If you're looking for top-rated counseling centers in Houston specializing in cognitive behavioral therapy for nurse burnout, Riaz Counseling is an excellent choice. We focus on providing effective mental health strategies tailored to the unique challenges faced by healthcare professionals to help you manage stress and recover from burnout.
If you are experiencing burnout symptoms, seeking professional mental health support is a proactive step. A therapist can help you develop coping mechanisms using approaches like cognitive behavioral therapy. To connect with a professional who understands the unique pressures of health care and nurse burnout, please reach out to us at Riaz Counseling through our contact form.
To recover from nurse burnout, focus on practical coping strategies. Prioritize work-life balance by setting boundaries, practice stress reduction techniques like mindfulness, and seek peer support. Also, consider professional development opportunities to reignite your passion. These burnout prevention steps are key to restoring your well-being.
While building personal resilience is helpful, it alone cannot prevent nurse burnout. Burnout is often a systemic issue rooted in the work environment. True burnout prevention requires organizational changes, emotional support systems, and a culture that values the well-being of the nursing profession, not just individual toughness.
Nurses in Houston facing burnout can access several support resources. Many hospitals offer Employee Assistance Programs (EAPs) with mental health services. Additionally, local professional organizations and counseling centers provide specialized support for nurse burnout. Seeking out these local resources is a great first step toward recovery.
If you feel that you or someone you know, may benefit from therapy, please reach out to our office for a FREE 15 minute consultation: LINK
Stay informed about the latest research in psychology.
.png)
Explore how Internal Family Systems (IFS) therapy heals trauma and restores self-leadership.
.png)
Explore how Internal Family Systems (IFS) therapy heals trauma, anxiety, and inner conflict.
.png)
A practical guide to recognizing, preventing, and healing teacher burnout in Houston schools.