
Suicide is a serious public health concern that leaves a lasting impact on families and entire communities. The good news, however, is that it is preventable. Improving mental health and preventing suicide requires a comprehensive approach that involves every level of society. You don't have to be an expert to make a difference. By learning more about suicide prevention, understanding the warning signs, and knowing how to offer support, you can become a vital part of the solution and help save lives.
Suicide is one of the leading causes of death in the United States, making it an urgent public health problem with far-reaching consequences. The loss from suicide affects not only individuals but also their families, friends, and communities, creating ripples of grief and trauma.
Understanding the scope of this issue is the first step toward effective prevention. By examining suicide data and trends, we can identify which groups are at a higher risk of suicide and develop targeted strategies. The most effective strategies for suicide prevention involve a multi-layered approach, from individual support to broad community programs.
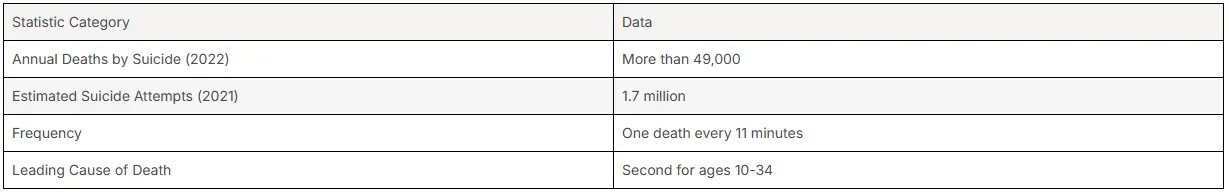
The rates of suicide in the United States are alarmingly high. According to the Centers for Disease Control and Prevention (CDC), more than 49,000 people died by suicide in 2022, which translates to one death every 11 minutes. It is the second leading cause of death for individuals between the ages of 10 and 34.
These suicide statistics highlight the need for a robust national response. Men are more than three times as likely as women to die by suicide, and the highest rates are seen in adults aged 75 and older. Firearms are the most common method, used in approximately half of all suicides.
National strategies recommended by organizations like the CDC focus on a comprehensive public health approach. This includes teaching coping skills, strengthening economic supports, promoting healthy connections, and improving access to suicide care. The Suicide Prevention Resource for Action from the CDC is a key resource that outlines these evidence-based approaches for states and communities to implement.
While national suicide data provides a broad overview, understanding trends at the state and local levels is crucial for targeted public health efforts. Suicide rates in Texas and major cities like Houston reflect the larger national crisis, requiring dedicated local resources and prevention programs. Specific local data helps communities tailor their interventions to meet the needs of their populations.
Are there specific suicide prevention resources available in Texas? Yes, the state has numerous initiatives and local organizations focused on mental health and suicide prevention. These resources aim to provide support, education, and crisis intervention to residents across Texas.
To understand the context of the national issue, here are some key statistics for the United States from the CDC:
The emotional impact of a suicide death is profound and long-lasting, extending far beyond the immediate family. For families, the loss can bring a complex mix of grief, guilt, anger, and confusion. This experience can strain relationships and create significant mental health challenges for survivors, who may themselves face an increased risk of suicide.
Communities also feel the effects. A suicide can send shockwaves through schools, workplaces, and neighborhoods, creating a sense of collective loss and fear. The social fabric of a community is weakened when it loses a member, and the event can trigger distress in others who may be vulnerable. This highlights why suicide is considered a major public health issue.
Because the effects are so widespread, community-wide suicide prevention is essential. Families can support loved ones by creating an environment of open communication, learning the warning signs, and knowing how to connect them with professional help. This supportive network is a critical component in preventing future tragedies.
Certain characteristics, known as risk factors, can make it more likely that an individual will consider, attempt, or die by suicide. These factors span individual, relationship, and societal levels and often combine to increase a person's suicide risk. Common risk factors include mental illness, substance abuse, and a history of trauma.
It's important to remember that risk factors are not the same as warning signs, which indicate an immediate risk. Understanding both can help you recognize when someone is struggling. While risk factors increase vulnerability, protective factors can help to offset this risk and build resilience.
Mental health disorders are closely linked to suicide risk. Conditions like depression, bipolar disorder, and anxiety disorders can cause immense emotional pain and feelings of hopelessness, which may lead to suicidal thoughts. The American Psychiatric Association notes that suicide is particularly linked to depression and alcohol use disorders.
However, a surprising finding from the CDC revealed that about 54% of people who died by suicide did not have a known mental health condition. This doesn't mean mental health wasn't a factor; many may have been struggling with undiagnosed challenges. This underscores the complexity of suicide and shows that it's not always tied to a formal diagnosis.
Mental health professionals play a critical role in addressing these risks. They are trained to assess for mental health disorders, provide evidence-based treatments, and manage suicide risk directly. Through therapy and support, they help individuals manage their symptoms and develop coping strategies, significantly reducing the risk of suicide.
Substance abuse is a major contributor to suicide risk. The use of drugs and alcohol can impair judgment, increase impulsivity, and deepen feelings of depression and hopelessness. Individuals with substance use disorders are at a particularly high risk, as these conditions often coexist with other mental health challenges.
Problematic substance use was identified by the CDC as a key factor contributing to suicide. Increased alcohol or drug use can also be a warning sign that someone is in immediate distress. The connection is so strong that reducing substance use through community-based practices is a recommended strategy for suicide prevention.
Counseling helps by addressing both the substance use and the underlying issues that contribute to it. Through therapies like Cognitive Behavioral Therapy (CBT), individuals can learn healthier ways to cope with stress and emotional pain. By treating substance use disorders, counseling directly tackles a significant risk factor and empowers individuals to regain control of their lives.
Living with a chronic illness or persistent pain can take a significant toll on a person's mental health. The daily challenges of managing a condition, coupled with physical discomfort, can lead to feelings of hopelessness, depression, and being a burden to others. These emotional struggles are recognized as a serious risk factor for suicide.
The connection between physical and mental health is undeniable. A CDC report highlighted chronic physical illness, including chronic pain, as a circumstance that can contribute to suicide. Effective pain management is therefore a crucial component of comprehensive healthcare and suicide prevention.
It is vital that healthcare providers address both the physical and emotional aspects of chronic conditions. Integrating mental health support into chronic illness care can help patients develop resilience and coping strategies. This holistic approach ensures that individuals receive the support they need to manage their health without succumbing to despair, playing a key role in suicide prevention.
Humans are social creatures, and a lack of connection can be detrimental to our well-being. Social isolation and loneliness are significant risk factors for suicide, as they can amplify feelings of hopelessness and despair. When people feel disconnected from others, they may believe that no one cares or that they have nowhere to turn for help.
Feeling like you don't belong or that you are a burden on others can be incredibly painful. Research confirms that these feelings, known as perceived burdensomeness and thwarted belongingness, are powerful predictors of suicide risk. Real-time studies have shown that loneliness can fluctuate and intensify, leading to spikes in suicidal ideation.
Conversely, strong social connections are powerful protective factors. Feeling connected to family, friends, and the community provides a sense of purpose and a critical support system during difficult times. Promoting healthy connections and engaging community members in shared activities are key strategies for suicide prevention that help combat the dangers of social isolation.
Economic and financial stress can place an immense burden on individuals and families, significantly increasing suicide risk. Job loss, overwhelming debt, or the inability to provide for one's family can lead to feelings of failure, shame, and hopelessness. These economic stressors are recognized as important risk factors that can contribute to a crisis.
A sudden financial loss or ongoing difficulty can feel like a catastrophic event, leaving people unable to see a way out. The CDC identifies improving household financial security and stabilizing housing as key suicide prevention strategies. Providing temporary assistance and economic supports can help people manage these challenges before they become overwhelming.
Addressing these risk factors is a critical part of a public health approach to suicide prevention. By expanding options for assistance and strengthening economic supports, communities can create a safety net for those in need. This helps reduce the desperation that financial stress can cause and allows individuals to focus on finding solutions rather than feeling trapped.
While risk factors indicate long-term vulnerability, warning signs signal an immediate risk of a suicide attempt. These are observable cues in a person’s behavior, speech, or mood that suggest they are having suicidal thoughts. Recognizing these signs is one of the most important things you can do to help.
Knowing what to look for allows you to take action and connect someone with the help they need. The Suicide Prevention Resource Center and other organizations emphasize that paying attention to these changes can be lifesaving. Let's look at some of the most common warning signs.
Significant changes in a person's behavior can be a clear indication of suicide ideation or intent. These shifts are often out of character and suggest that someone is in deep distress. Paying attention to these actions is a key aspect of behavioral health monitoring and suicide prevention.
Families can support loved ones by being vigilant for these changes and not dismissing them as just a phase. Such suicidal behavior may include preparing for death, such as writing a will, giving away prized possessions, or saying goodbye to friends and family.
Other alarming behavioral signs include:
What a person says can be one of the most direct warning signs of their suicidal thoughts. Listen carefully if someone begins talking or writing about death, dying, or suicide. These expressions should always be taken seriously, as they are often a cry for help.
A deep sense of hopelessness is a common thread in many of these verbal cues. You might hear comments about feeling worthless, helpless, or having no reason to live. Phrases like "It would be better if I wasn't here" or "I just want out" are red flags that indicate a high suicide risk.
Another common theme is the feeling of being a burden to others or feeling trapped with no way out. These expressions reveal a dangerous state of mind where suicide may seem like the only solution. If you hear someone you care about saying these things, it's time to ask directly if they are thinking about suicide.
Dramatic and sudden mood swings can be a concerning warning sign of increased suicide risk. This might look like a shift from extreme sadness to unexpected calmness or even happiness. This sudden sense of peace can sometimes mean the person has made a decision to end their life and feels a sense of relief, which is highly dangerous.
Another critical sign is withdrawal. If someone you know starts pulling away from friends, family, and social activities they used to enjoy, it could be a symptom of depression or suicidal thinking. This social withdrawal often accompanies feelings of isolation and can make it harder for them to seek help.
These changes in mood and behavior should not be ignored. They often signal that a person is struggling with intense emotional pain. Reaching out and letting them know you are there for them can break through the isolation and be the first step toward getting them the support they need.
Disruptions in a person's routine, especially their sleep patterns, can be indicators of poor mental health and potential risk factors for suicide. Sleeping too much or too little is a common symptom of depression and other mental health conditions linked to suicide. These sleep changes can worsen mood and impair judgment.
Similarly, a noticeable change in daily activities can be a red flag. This could include neglecting personal hygiene, a loss of interest in work or hobbies, or a significant change in appetite. These shifts suggest that the person may be struggling to cope with their daily life due to underlying emotional distress.
When combined with other warning signs, these changes in sleep and daily activities paint a picture of someone who is not doing well. Paying attention to these seemingly small details is important, as they can be part of a larger pattern of risk. Offering support and encouraging them to see a professional can make a significant difference.
Just as risk factors increase the likelihood of suicide, protective factors do the opposite—they make it less likely. These are characteristics or conditions that build resilience and help buffer individuals from suicidal thoughts and behaviors. Strengthening these factors is a core part of any effective suicide prevention strategy.
Protective factors can include strong support networks, access to care, and personal coping skills. Communities can implement comprehensive suicide prevention programs by focusing on building these assets. By fostering community support and ensuring resources are available, we create an environment where people are less likely to fall into crisis.
Having strong social connections is one of the most powerful protective factors against suicide. Feeling connected to family, friends, and social institutions gives people a sense of belonging and purpose. These relationships provide emotional support and a safety net during times of stress.
Community support plays a vital role in fostering these connections. When communities promote healthy peer norms and engage members in shared activities, they create an environment where people feel valued and included. This sense of belonging directly counters the dangerous feelings of isolation and loneliness that often accompany suicidal thoughts.
Building these support systems is a proactive suicide prevention strategy. It involves more than just individual relationships; it includes creating a culture of care within schools, workplaces, and neighborhoods. By strengthening the social fabric, we help ensure that no one has to face their struggles alone.
Easy access to effective and affordable healthcare is a critical protective factor in suicide prevention. When people can get help for mental and physical health issues, they are better equipped to manage conditions that might increase their suicide risk. This includes having mental health conditions covered by health insurance policies and having enough providers available, especially in underserved areas.
Counseling helps prevent suicide by providing individuals with a safe space to address their struggles. Mental health professionals use evidence-based interventions to help people manage suicidal thoughts, develop coping skills, and address underlying disorders like depression or anxiety.
Quality healthcare and counseling offer several benefits that act as protective factors:
The ability to manage challenges and resolve conflicts is a powerful skill that supports good mental health. When people feel equipped to handle life's stressors, they are less likely to feel overwhelmed and hopeless. Developing strong problem-solving skills is therefore a key protective factor against suicide.
These skills can be taught and learned at any age. The CDC recommends teaching coping and problem-solving skills as a core suicide prevention strategy. This can be done through social-emotional learning programs in schools or parenting skills training that improves family relationships. Such education helps build resilience from a young age.
By empowering individuals with the tools to navigate difficulties, we help them see that problems are manageable and that there are alternatives to suicide. This proactive approach focuses on building strength and self-efficacy, making people less vulnerable when they face personal, financial, or relational crises.
A person's cultural and religious beliefs can serve as significant protective factors against suicide. Many belief systems emphasize the value of life and may include prohibitions against suicide, which can act as a powerful deterrent for individuals in distress. These beliefs can provide a sense of hope, purpose, and meaning.
Having a strong sense of cultural identity can also be protective. It connects individuals to a community with shared values and traditions, fostering a sense of belonging and support. This connection can be a source of strength and resilience, particularly for those facing historical or personal trauma.
These beliefs often come with built-in support networks, such as faith communities, that can rally around a person in crisis. The shared values and social support found within these groups reinforce the idea that life is worth preserving. For these reasons, cultural and religious beliefs are recognized as important protective factors in suicide prevention.
The most effective suicide prevention strategies are evidence-based and part of a comprehensive public health approach. These best practices have been studied and shown to work in reducing suicidal behaviors and deaths. They move beyond simply reacting to crises and focus on proactive, multi-level interventions.
These strategies, highlighted by organizations like the CDC and the National Action Alliance for Suicide Prevention, include everything from strengthening economic supports to providing better suicide-specific care. Let's explore some of the key evidence-based strategies that form the foundation of modern suicide prevention efforts.
Identifying individuals at risk before they reach a crisis point is a cornerstone of effective suicide prevention. Early identification involves training "gatekeepers"—such as teachers, doctors, and community leaders—to recognize warning signs and ask directly about suicide. This allows for intervention before a person's distress becomes unmanageable.
Once someone is identified as being at risk or in a crisis, immediate intervention is crucial. This can involve creating a safety plan, connecting them with professional help, or providing support through a crisis line like 988. Crisis intervention aims to de-escalate the situation and ensure the person's immediate safety.
This public health approach emphasizes that everyone has a role to play. By equipping more people with the skills for early identification, we create a wider safety net. Prompt and compassionate crisis intervention can be the turning point that helps a person navigate their darkest moments and find a path toward recovery.
To effectively identify people at risk, healthcare systems are increasingly adopting comprehensive screening practices. This involves systematically asking all patients about suicidal thoughts, rather than waiting for them to disclose this information. This proactive approach helps catch risk that might otherwise be missed.
Validated tools are used to make this process consistent and reliable. The Columbia-Suicide Severity Rating Scale (C-SSRS) is one such instrument. It helps clinicians and trained individuals gauge the severity and immediacy of suicide risk by asking specific questions about suicidal ideation and behaviors. Its use has been shown to predict future suicide attempts.
Effective screening practices should:
For individuals struggling with suicidal thoughts and behaviors, certain psychosocial treatments have been proven effective. These therapies go beyond just treating underlying disorders and target suicidal behavior directly. Randomized controlled trials have shown that these interventions can significantly reduce suicide attempts and reattempts.
Two of the most well-known evidence-based treatments are Dialectical Behavior Therapy (DBT) and Cognitive Therapy (also known as Cognitive Behavioral Therapy or CBT). DBT teaches skills for managing intense emotions and distress, while CBT helps individuals change the negative thought patterns that contribute to suicidal feelings. Both have a strong evidence base for reducing suicidality.
The Collaborative Assessment and Management of Suicidality (CAMS) is another suicide-specific intervention that has shown positive results. Widespread implementation of these psychosocial treatments is a key goal in suicide prevention, as they provide individuals with the concrete skills needed to stay safe and build a life worth living.
One of the most effective and immediate ways to prevent suicide is to reduce access to lethal means. This strategy involves making it more difficult for a person in crisis to access methods of suicide, such as firearms, medications, or high places. Creating time and distance between a suicidal thought and the means to act on it can save a life.
Many suicides are impulsive. If a highly lethal method is not readily available, the person may not attempt suicide, or may use a less lethal method that they are more likely to survive. This provides a crucial window of opportunity for the impulse to pass or for help to arrive. Studies have shown that restricting access to lethal means, like securing firearms or changing packaging for medications, leads to a decrease in suicide deaths.
This strategy is a key part of safety planning. It involves talking openly with individuals at risk about the means they have considered and collaborating on ways to secure them. Resources like the CALM (Counseling on Access to Lethal Means) training help clinicians and others have these important conversations.
Suicide prevention isn't just the responsibility of healthcare providers; it requires a community-wide effort. Community-based approaches focus on creating a social environment that promotes mental wellness and provides strong support networks. These programs aim to build awareness, reduce stigma, and foster a culture where seeking help is encouraged.
How can communities implement comprehensive suicide prevention programs? They can do so by educating the public, creating safe and supportive environments, strengthening local connections, and empowering peers to help one another. Let's look at how these strategies work together to build a resilient community.
Increasing public awareness is a foundational step in all suicide prevention efforts. Education programs can teach people to recognize the warning signs of suicide, challenge myths and stigma, and know how to connect someone to help. When more people are informed, the entire community becomes safer.
These programs can take many forms. Schools can implement social-emotional learning curricula that teach students coping and problem-solving skills from a young age. Workplaces and community organizations can host gatekeeper trainings that empower employees and members to intervene when they see someone struggling.
The goal of these public health initiatives is to create a culture of prevention. By normalizing conversations about mental health and suicide, we make it easier for people to seek help for themselves and to offer it to others. This collective awareness is a powerful tool for saving lives.
Creating protective environments is a key strategy in any comprehensive suicide prevention program. This means shaping our physical and social surroundings to promote safety and well-being, especially for vulnerable groups who may be at higher risk. A safe environment reduces opportunities for self-harm and fosters a sense of security.
This can be done in many ways. At a broad level, it includes policies that reduce access to lethal means. In specific settings like schools or workplaces, it involves creating a healthy organizational culture that is supportive, inclusive, and free from bullying or harassment.
A safe environment for vulnerable groups includes:
Strong support networks are powerful protective factors against suicide, and these networks are built at the local level. Strengthening these connections involves fostering a sense of community where people feel they belong and can rely on one another during difficult times. This is a core function of community-based suicide prevention.
Local organizations, such as faith communities, clubs, and volunteer groups, play a crucial role in building these support networks. They provide opportunities for shared activities and social interaction, which combat the loneliness and isolation that can increase suicide risk. Collaboration between these groups and mental health services can create a seamless web of support.
By promoting healthy peer norms and encouraging community engagement, we can help ensure that individuals have multiple sources of support to turn to. A person connected to a strong local network is less likely to feel alone with their problems and more likely to find the help they need.
Peer support initiatives are an increasingly recognized and effective component of community support for suicide prevention. These programs connect individuals who have shared life experiences, such as struggles with mental health or suicidal thoughts, allowing them to support each other in a way that professionals cannot.
The power of peer support lies in mutual understanding and empathy. Speaking with someone who has "been there" can reduce feelings of shame and isolation, making it easier for a person at suicide risk to open up. A peer support intervention in India, for example, led to a significant decrease in suicide attempts.
These initiatives are valuable protective factors because they build a sense of community and hope. Peers can help each other navigate the healthcare system, practice coping skills, and provide ongoing encouragement. By developing and investing in peer support programs, communities can harness the power of shared experience to save lives.
Families and caregivers often find themselves on the front lines of suicide prevention. Their close relationship with an individual at risk puts them in a unique position to notice warning signs and provide immediate support. Open communication and a willingness to get involved are crucial family roles in this process.
So, how can families support loved ones who may be at risk of suicide? They can do so by learning how to talk openly about suicide, creating a safe home environment, and knowing how to connect their loved one to professional support services. Let's examine these vital actions more closely.
One of the most important things families can do for suicide prevention is to foster open and honest communication. This means creating a safe space where a loved one feels comfortable sharing their struggles without fear of judgment. It starts with being willing to have difficult conversations.
A common fear is that asking about suicide will plant the idea in someone's head. However, studies show this is not true. In fact, directly asking, "Are you thinking about suicide?" can be a relief for the person struggling and is the first step in getting them help. The 988 Suicide & Crisis Lifeline recommends this as a key action.
To communicate effectively with a loved one, families can:
Creating a safe home environment is a practical and life-saving step that families can take. This is a core component of safety planning, which is a collaborative process to help an individual get through a suicidal crisis. A key part of this plan involves reducing access to lethal means within the home.
This means thinking about and securing any items that could be used for self-harm, especially those the person has mentioned in their suicide plan. This could involve locking up firearms, storing medications securely, or removing sharp objects. Reducing access to these risk factors creates a vital buffer of time and space, allowing the suicidal urge to pass.
Families can work with their loved one and a mental health professional to develop a comprehensive safety plan. This written plan outlines warning signs, coping strategies, and people to contact during a crisis. It empowers both the individual and their family with a clear set of actions to take to maintain safety.
For families, being able to recognize the warning signs of suicide risk is the first step toward taking life-saving action. As we've discussed, these signs can be verbal, behavioral, or mood-related. Paying close attention to changes in your loved one is essential for early intervention.
Once you recognize these signs, the next step is to act. Don't wait or assume it will pass. The 988 Lifeline outlines five action steps, which include asking directly about suicide and then being there for the person. This means showing your support, listening to them, and reminding them that they are not a burden.
The ultimate goal of these action steps is to keep them safe. This involves the safety planning we've just covered, as well as helping them connect with ongoing support. Your presence and decisive action can make all the difference in a moment of crisis.
A crucial way families can support loved ones is by helping them connect to professional support services. You don't have to be their therapist; your role is to be a bridge to the mental health services that can provide expert care. This might involve helping them make an appointment or offering to go with them.
The 988 Suicide & Crisis Lifeline is an excellent starting point. By calling or texting 988, you and your loved one can be connected to a trained crisis counselor 24/7. They can provide immediate support and direct you to local mental health resources. Making this connection is a vital part of suicide prevention.
Finally, follow up. After the initial crisis has passed, checking in with your loved one lets them know you are still there for them. This ongoing support encourages treatment engagement and reinforces that they are not alone on their journey to recovery. This is a powerful way families can contribute to long-term safety.
Mental health professionals are specialists in suicide prevention, equipped with the training and tools to assess and manage the risk of suicide. Their role is to provide evidence-based counseling and treatment that directly targets suicidal thoughts and behaviors, helping patients find a path to recovery.
They play a multifaceted role that extends from individual patient care to broader advocacy. From conducting thorough risk assessments to implementing follow-up protocols, mental health professionals are central to creating a system of care that aims for zero suicides among patients. Let's explore their key responsibilities.
A primary role of mental health professionals is to conduct thorough assessments of suicide risk in their patients. This goes beyond just asking about suicidal thoughts and involves a comprehensive evaluation of risk and protective factors. This systematic screening is essential for determining the appropriate level of care.
To do this, professionals use validated tools and guidelines. The Suicide Assessment Five-step Evaluation and Triage (SAFE-T) pocket card, for example, guides clinicians through a process of identifying risk factors, inquiring about suicidal plans, and determining risk level. This structured approach ensures that the assessment is thorough and consistent.
A comprehensive risk assessment by mental health professionals typically includes:
Once a patient's suicide risk is assessed, mental health professionals provide patient-centered counseling designed to reduce that risk. This means tailoring the treatment to the individual's specific needs and collaborating with them to set goals. This approach empowers the patient and makes them an active participant in their own recovery.
This counseling often involves evidence-based psychosocial treatments that have been proven effective in suicide prevention. Therapies like Dialectical Behavior Therapy (DBT) and Cognitive Behavioral Therapy (CBT) help patients develop skills to manage distressing emotions and change harmful thought patterns. The focus is on building a life that feels worth living.
Ultimately, patient-centered care is about building a strong, trusting therapeutic relationship. In this safe environment, patients can explore the drivers of their suicidal feelings and learn new ways to cope. This collaborative and compassionate approach is at the heart of effective counseling for suicide prevention.
Continuity of care is critical in suicide prevention, especially during high-risk periods like after a discharge from an emergency department or hospital. Mental health professionals and health care systems play a key role in implementing follow-up care protocols to ensure patients don't fall through the cracks.
These protocols can include simple but effective interventions. Follow-up phone calls, letters, or text messages after a crisis have been shown to reduce suicidal behaviors and deaths. These contacts provide a sense of connection and support, reminding the individual that someone cares and that help is still available.
A "warm handoff" is another important practice, where a provider directly connects a patient to their next point of care, rather than just giving them a phone number. This ensures a smoother transition and increases the likelihood that the patient will engage in follow-up treatment. These protocols are a vital part of a coordinated health care system focused on suicide prevention.
The role of mental health professionals in suicide prevention extends beyond individual patient care. They are also powerful advocates for policy improvements that can create a better public health landscape for mental wellness. Their expertise and firsthand experience give them a unique voice in shaping policy.
One key area of advocacy is improving access to care. This includes pushing for health insurance policies that provide comprehensive coverage for mental health conditions, on par with physical health. They can also advocate for increased funding for mental health services to ensure there are enough providers, especially in underserved areas.
By engaging in advocacy, mental health professionals can help address the systemic issues that contribute to suicide risk, such as lack of access to care and stigma. Their work on policy improvements helps build a society that is more supportive of mental health, benefiting everyone.
Are there specific suicide prevention resources available in Texas? Yes, the state is home to a range of suicide prevention programs aimed at providing mental health support and reducing suicide rates. These programs reflect the broader national strategies, applying them at the state and local levels to meet the unique needs of Texans.
These initiatives are part of a larger public health effort involving state agencies, local organizations, and community leaders. From statewide mental health support to school-based programs, Texas is working to build a comprehensive network of care. Let's explore some of the types of resources you can find in the state.
Texas has implemented several statewide initiatives to bolster mental health support and create a robust suicide prevention program. These efforts often align with the strategies recommended by the CDC, focusing on a comprehensive public health approach. This includes strengthening economic supports, promoting healthy connections, and improving the delivery of suicide care.
These statewide programs aim to create a coordinated system of care. This might involve expanding access to mental health services in rural and underserved areas through telehealth, or integrating mental health screenings into primary care settings across Texas. The goal is to make it easier for anyone, anywhere in the state, to get the help they need.
Another key component is public awareness campaigns. These initiatives work to reduce the stigma surrounding mental illness and suicide, encouraging Texans to seek help and look out for one another. By promoting a message of hope and help, these statewide programs aim to change the conversation around suicide.
In a large metropolitan area like Houston, a wide array of community resources is available for suicide prevention. These local organizations and mental health services provide direct support to residents, from crisis intervention to long-term counseling. Knowing where to find these resources is key for anyone seeking help.
So, where can someone in Houston find mental health counseling for suicide prevention? A great first step is to contact the 988 Suicide & Crisis Lifeline. They can provide immediate support and connect you to local resources in the Houston area. Many universities, non-profits, and healthcare systems also offer mental health services.
Some types of community resources you can find in Houston include:
Schools are a critical setting for suicide prevention, as they are central to the lives of young people. School-based prevention programs in Texas and across the country aim to equip students with the skills they need to navigate life's challenges and to create a supportive school environment where students feel safe seeking help.
These programs often include social-emotional learning (SEL) curricula, which teach students skills like problem-solving, conflict resolution, and emotional regulation. By building these protective factors from a young age, schools can help foster resilience and reduce the risk of future mental health crises.
Another key component is training for teachers and staff. These "gatekeeper" trainings teach educators to recognize the warning signs of suicide in young people and how to connect them with school counselors or other mental health professionals. This creates a safety net within the school, ensuring that struggling students are identified and supported.
Effective suicide prevention relies on strong collaboration between various local organizations. No single entity can tackle this public health issue alone. When government agencies, healthcare providers, schools, non-profits, and community groups work together, they can create a more comprehensive and effective safety net.
This collaboration allows for a pooling of resources and expertise. For example, a local mental health center might partner with a school district to provide on-site counseling services. A faith community might work with a local chapter of the American Foundation for Suicide Prevention to host an awareness event.
These partnerships are essential for reaching all corners of a community. They help ensure that suicide prevention messages and resources are culturally competent and accessible to everyone, including vulnerable and hard-to-reach populations. This coordinated effort is the hallmark of a strong, community-based public health approach to suicide prevention.
Counseling and mental health services are the cornerstones of professional intervention for suicide prevention. These services provide a structured, supportive environment where individuals can work through the issues contributing to their suicidal thoughts with a trained professional.
So, how does counseling help in preventing suicide? It does so by providing evidence-based treatments that teach coping skills, address underlying mental health conditions, and help individuals develop a sense of hope for the future. Let's delve into the types of counseling available and the benefits of seeking professional help.
There are several types of counseling that have been specifically studied and found to be effective for suicide prevention. These are not just generic "talk therapies"; they are structured approaches that directly target the thoughts, feelings, and behaviors associated with suicide.
Two of the most effective are Cognitive Therapy (CBT) and Dialectical Behavior Therapy (DBT). Randomized controlled trials have shown that both of these therapies can significantly reduce suicide attempts. They focus on teaching practical skills that patients can use to manage their distress and stay safe.
Other effective or promising types of counseling for suicide prevention include:
Finding mental health services in a large city like Houston can feel overwhelming, but there are several pathways to get connected with care. The goal is to find a provider or service that fits your needs and provides easy access to support, especially when you are in distress.
A great starting point for anyone is the 988 Suicide & Crisis Lifeline. By calling, texting, or chatting online, you can get immediate, confidential support and be referred to local mental health services in the Houston area. This is a free and accessible resource available 24/7.
Other avenues include asking your primary care doctor for a referral, checking with your health insurance provider for a list of in-network therapists, or contacting local university psychology clinics, which often provide low-cost services. Many non-profit organizations in Houston also offer counseling and support for suicide prevention.
Seeking professional intervention for suicidal thoughts is a sign of strength, and the benefits are life-saving. Mental health professionals are trained to provide a level of care that friends and family, however well-meaning, cannot. They offer a structured, evidence-based approach to suicide prevention.
One of the primary benefits is the development of a collaborative safety plan. A therapist can help you identify your personal warning signs and create a detailed plan of coping strategies and support contacts to use during a crisis. This provides a clear roadmap for staying safe.
Furthermore, mental health professionals can diagnose and treat underlying conditions like depression or anxiety that may be contributing to your suicidal feelings. Through therapies proven to work, they help you build long-term skills for emotional regulation and problem-solving, leading to lasting improvements in your well-being and a reduction in suicide risk within the broader context of health care.
In today's digital world, telehealth has become an invaluable tool for providing immediate help and increasing access to mental health services for suicide prevention. Telehealth allows you to connect with a mental health professional remotely, using a phone or computer, which can be crucial during a crisis or for those who face barriers to in-person care.
This remote access to care means that help is often just a click or a call away. The 988 Suicide & Crisis Lifeline is a prime example, offering immediate help through phone calls, texts, and online chat at 988lifeline.org. These services are free, confidential, and available 24/7.
Telehealth options for mental health services and suicide prevention include:
Suicide is the second leading cause of death for young people aged 10-34, making youth and teen suicide prevention a top priority. While the core principles of prevention are similar across all ages, the approaches for teens must be tailored to their unique developmental stage, social worlds, and risk factors.
So, is there a difference between suicide prevention approaches for adults and teens? Yes. Prevention for young people often places a greater emphasis on the roles of schools, peers, and parents. It requires understanding the specific pressures teens face and leveraging the systems of support that surround them.
Adolescents face a unique set of risk factors that can contribute to suicidal thoughts and behaviors. The teenage years are a time of significant brain development, social pressure, and identity formation, which can make them particularly vulnerable to mental health challenges.
One major risk factor for adolescents is bullying, both in person and online. The constant stress and social pain from bullying can lead to feelings of hopelessness and isolation. Academic pressure and failures are another significant stressor that can feel overwhelming to a young person.
Other risk factors unique to or more pronounced in this age group include relationship breakups, family conflict, a history of trauma or abuse, and exposure to the suicidal behavior of others. Understanding these specific risks is crucial for parents, educators, and anyone involved in youth suicide prevention.
Schools are a vital setting for suicide prevention, and school programs that incorporate peer support can be particularly effective for young people. Teens are often more likely to talk to their friends about their struggles than to an adult, so empowering peers with the right skills is essential.
These school programs focus on creating a supportive and informed student body. They might involve educating students on the warning signs of suicide and teaching them how to connect a friend with a trusted adult, like a school counselor. This builds a culture of students looking out for one another.
Effective school and peer support programs often include:
Effective suicide prevention for teens requires strategies that are tailored to their specific needs and social context. A one-size-fits-all approach that works for adults may not resonate with young people. This means using language, technology, and intervention methods that are relevant to their lives.
For example, prevention strategies for teens often leverage technology, such as crisis text lines or mental health apps, as teens may be more comfortable seeking help this way. Family involvement is also key, and therapies like Cognitive-Behavioral Family Treatment have been developed specifically to address youth suicide attempts by involving the whole family.
Mental health professionals who work with teens must be skilled in building rapport with this age group and understanding their unique challenges. Evidence-based treatments like Dialectical Behavior Therapy for Adolescents (DBT-A) have been adapted to be more effective for younger populations, addressing issues like impulsivity and emotional dysregulation within a family context.
Parents and educators are two of the most important groups of adults in a teen's life, and their engagement is crucial for effective suicide prevention. They are in a prime position to notice changes in behavior and to create a supportive environment that fosters mental well-being.
Educating parents on the warning signs of suicide and how to talk to their kids about mental health is a key strategy. Parenting skills programs can help improve family relationships and communication, which are strong protective factors. Similarly, training educators as "gatekeepers" ensures there is a safety net at school.
When parents and educators work together, they can provide a consistent and coordinated system of support for a young person. This collaboration ensures that if a teen is struggling, there are multiple adults in their life who are prepared to notice, listen, and connect them to the appropriate support services.
Support for adults and seniors in navigating their mental health is crucial for effective suicide prevention. Recognizing warning signs, such as withdrawal or changes in mood, can help identify individuals at risk. Implementing protective factors through strong support systems, including friends, family, and mental health professionals, enhances resilience against suicidal thoughts. Programs focused on promoting independence and mental wellness, like engagement in meaningful activities and access to mental health services, can empower older adults. Tailored interventions that meet their unique needs contribute to a comprehensive approach in reducing the risk of suicide while fostering a sense of belonging and positivity.
Various challenges often surface during midlife and late life, influencing the risk of suicide. Factors such as substance use, health issues, and major life changes can significantly impact mental health. It's also essential to recognize the elevated risks associated with unresolved grief and loneliness, which can lead to feelings of hopelessness. Additionally, mood disorders like depression and anxiety are prevalent in these age groups, often exacerbated by life transitions. Understanding these risk factors enables caregivers and health professionals to implement effective suicide prevention strategies, ultimately fostering environments that promote mental wellness and resilience among older adults.
A strong support system plays a vital role in enhancing the mental health of older adults. Family members, friends, and community resources can help alleviate feelings of isolation that often accompany aging. Health professionals, including social workers and mental health specialists, can provide valuable guidance on recognizing warning signs of suicidal thoughts and behaviors. Establishing connections through local support groups or mental health services offers older adults a sense of belonging and understanding. Implementing a comprehensive approach that includes emotional and social support is crucial for safeguarding their well-being and reducing the risk of suicide in this vulnerable population.
Targeted intervention strategies can significantly reduce the risk of suicide among different age groups. For younger individuals, fostering resilience through skills training and engaging in supportive environments can be vital. Programs utilizing cognitive therapy and peer support create a sense of belonging and safety. For older adults, addressing isolation and promoting healthy social connections are essential. Mental health professionals often recommend comprehensive approaches that include regular health check-ups and the involvement of family in care transitions. By customizing interventions based on age-specific needs, communities can effectively support individuals at risk, leading to improved mental wellness and reduced suicide rates.
Encouraging independence in older adults is pivotal for fostering mental wellness. Providing opportunities for engagement in community activities can significantly bolster self-esteem and improve overall outlook on life. Incorporating therapeutic practices, such as cognitive therapy and dialectical behavior therapy, offers invaluable support in managing emotional challenges. Additionally, establishing strong social connections serves as a protective factor against suicidal thoughts. When older adults feel embraced by their community and have access to mental health services, they are better equipped to navigate life's ups and downs, thus reducing the risk of suicide. This holistic approach is key to promoting resilience and emotional well-being.
A comprehensive approach to suicide prevention incorporates collaboration among various stakeholders—including health professionals, community organizations, and government agencies. By adhering to CDC recommendations, states develop tailored suicide prevention programs aimed at reducing risk factors and enhancing protective factors. Federal funding plays a vital role in expanding mental health services and implementing evidence-based interventions. National campaigns also raise awareness, encouraging open discussions and facilitating the identification of warning signs. Initiatives such as the Zero Suicide framework exemplify commitment to continuous improvement in health care systems, ultimately ensuring accessible support for individuals facing suicidal thoughts or behaviors.
A multifaceted approach is essential for effective suicide prevention, as highlighted by the CDC's recommendations and guidelines. Prioritizing mental health, these guidelines emphasize the importance of identifying risk factors and early intervention for individuals displaying warning signs, such as suicidal thoughts or behaviors. Collaboration among health professionals is crucial to ensure a continuum of care, particularly in primary care settings. The CDC also advocates for the integration of evidence-based practices, like cognitive therapy, and promotes awareness on lethal means safety. By implementing these strategies, communities can better support those at risk and reduce rates of suicide across the United States.
Substantial federal funding plays a crucial role in enhancing suicide prevention efforts across the United States. By supporting community programs and mental health services, this funding addresses risk factors associated with suicide, such as mental illness and substance use disorders. Investments in research and public health initiatives empower health professionals with the tools and resources needed to tackle suicide rates effectively. Additionally, by allocating resources to innovative programs like the Zero Suicide initiative, federal funding ensures that comprehensive approaches are implemented, fostering a supportive environment for those grappling with suicidal thoughts or behaviors.
Effective suicide prevention involves a collaborative approach that unites various agencies, including health care providers, mental health professionals, and community organizations. By sharing resources and information, these groups can create a supportive network that addresses the diverse needs of individuals at risk. This teamwork allows for comprehensive mental health services, ensuring that protective factors are identified and enhanced. Moreover, fostering partnerships enables the implementation of best practices, such as safety planning and continuity of care, which are crucial for reducing suicide rates. Together, these efforts can make a significant impact in supporting those affected by suicidal thoughts and behaviors.
National campaigns play a pivotal role in raising awareness about suicide prevention and mental health. By disseminating critical information, these initiatives help individuals recognize warning signs and understand available resources. Campaigns such as “Zero Suicide” and those led by the American Foundation for Suicide Prevention encourage community conversations, ultimately fostering protective factors against suicidal behavior. Collaborations with health care systems ensure that the message reaches diverse populations, including young adults and seniors, enhancing the accessibility of mental health services. The continuous engagement in these efforts significantly contributes to reducing stigma and improving suicide prevention outcomes across the United States.
In a crisis, immediate action is essential. Recognizing warning signs, such as sudden changes in behavior or expressions of hopelessness, can guide effective responses. Utilizing resources like the 988 Suicide & Crisis Lifeline provides quick, professional support. Creating a safe environment involves keeping lethal means away and ensuring those at risk know where to turn for help. Collaboration with mental health professionals and crisis intervention teams strengthens the response, fostering a network of support. Encouraging open conversations about mental health and suicidal thoughts helps reduce stigma, promoting a culture of understanding and empathy.
In an emergency involving suicidal thoughts or actions, swift and compassionate responses are crucial. First, ensure the person's immediate safety by removing any lethal means, like sharp objects or medications. Engage them in conversation, actively listening to their feelings and concerns. Encourage them to seek professional help and provide information about local mental health services. Calling emergency services or a suicide crisis hotline can connect them with trained professionals. Following these steps can significantly lower the risk of a suicide attempt and provide a supportive environment for healing and recovery.
An essential resource, the 988 Suicide & Crisis Lifeline offers immediate support for those grappling with suicidal thoughts or crises. Accessible 24/7, trained counselors provide empathetic listening and effective strategies, fostering a safe space to explore emotions and challenges. This lifeline not only connects individuals with mental health professionals but also promotes continuity of care by facilitating referrals to local services and community resources. As a vital part of public health initiatives, this service encourages open conversations around mental health, reduces stigma, and ultimately helps lower suicide rates across the United States.
Crisis intervention teams in Houston play a crucial role in addressing mental health emergencies, especially for those experiencing suicidal thoughts. These specialized groups, consisting of law enforcement and mental health professionals, provide immediate support and assessment in high-stress situations. By focusing on de-escalation and connection to appropriate services, they reduce the risk of suicide and enhance safety. Their approach promotes understanding of warning signs and risk factors while offering resources tailored to individuals’ needs. This collaborative method ensures that care transitions are smooth, paving the way for continued mental health support and overall well-being for those in crisis.
Following a crisis, providing ongoing support is essential for recovery. Creating a safe environment can significantly reduce the risk of suicide and help individuals regain their sense of stability. Mental health professionals may suggest regular check-ins and utilize evidence-based practices, such as safety planning, to address suicidal thoughts and promote coping strategies. Encouraging participation in social activities can enhance protective factors and lessen feelings of isolation. Access to comprehensive mental health services, including cognitive therapy and peer support, empowers individuals to navigate their emotions while reinforcing their resilience and overall well-being. Practicing empathy can truly make a difference.
Advocacy plays a crucial role in shaping effective public policy aimed at suicide prevention. Engaging with legislators helps promote legislation that supports mental health services, increases funding for suicide prevention programs, and raises awareness about warning signs. Grassroots efforts, like community outreach, empower individuals to become advocates, fostering a supportive environment that reduces stigma around mental illness. Collaborating with health professionals and organizations, such as the American Foundation for Suicide Prevention, amplifies voices that strive for meaningful change. Together, these initiatives create a comprehensive approach to addressing the risk of suicide, ultimately promoting mental wellness for all.
Legislative action plays a vital role in enhancing suicide prevention efforts across the United States. By supporting bills that fund mental health services and establish comprehensive suicide prevention programs, communities can significantly reduce the risk of suicide. Encouraging lawmakers to prioritize mental health resources ensures that health professionals have the tools necessary to provide effective care. Moreover, implementing educational initiatives about risk factors and warning signs through state-sponsored campaigns can foster awareness and promote protective factors. Together, these measures can pave the way for a safer, more supportive environment for those facing suicidal thoughts.
Building a network of community awareness in Texas is crucial for enhancing mental health and addressing the high rates of suicide. Educational initiatives can empower residents to recognize warning signs of suicidal behavior and initiate conversations about mental health. Local events can promote resources such as mental health services and suicide prevention programs, while social media campaigns can spread vital information quickly. Collaborating with schools, health professionals, and community organizations allows for a consistent message about mental wellness and protective factors. Together, we can foster an environment that encourages open dialogue, reduces stigma, and ultimately saves lives.
Endless stereotypes surrounding mental health inhibit open conversation about suicide prevention. Anti-stigma campaigns play a critical role in reshaping perceptions and encouraging individuals to seek help. By fostering environments where mental health issues are openly discussed, these initiatives promote understanding and empathy among communities. Health professionals and social workers can collaborate on these efforts, providing resources and education that highlight the importance of support and acceptance. With such supportive frameworks, those with suicidal thoughts feel empowered to reach out, ultimately aiding in reducing the risk of suicide and facilitating better mental health outcomes for everyone.
Engaging citizens in suicide prevention efforts empowers communities and fosters a sense of connection. Volunteer opportunities abound, from local mental health advocacy groups to national organizations. Individuals can participate in training programs that teach effective communication skills, helping to identify warning signs and provide support. By attending community events or workshops, volunteers can raise awareness about mental health resources and promote protective factors. This involvement not only enhances personal growth but also strengthens support networks essential for those at risk of suicide. Each effort contributes significantly to creating a healthier community focused on prevention and understanding.
Fostering a society that prioritizes mental health is essential for effective suicide prevention. By understanding the nuances of risk and protective factors, we can create a robust support system for adults and seniors alike. Engaging in comprehensive programs and utilizing evidence-based strategies can significantly reduce suicide rates. Community involvement and advocacy play vital roles in building awareness, combating stigma, and ensuring that resources are accessible. Every individual can contribute to this mission, paving the way for a brighter, healthier future that nurtures mental wellness and supports those in crisis. Together, we can make a difference!
To help a family member who may be suicidal, approach them with empathy and concern. Encourage open dialogue about their feelings, listen actively, and avoid judgment. Suggest professional help and offer to accompany them to appointments or support groups for reassurance and connection.
If someone expresses intent to harm themselves or shows severe warning signs, contact professional help or emergency services immediately. Riaz Counseling is available to provide urgent support and guide you through the process safely.
In Houston, Riaz Counseling offers vital support for individuals in crisis, providing professional guidance and therapeutic interventions. Their trained counselors specialize in crisis management to help clients navigate difficult emotions and situations effectively. Seeking help from local resources can be a crucial step towards healing.
Families can support loved ones at risk of suicide by fostering open communication, offering non-judgmental listening, and encouraging professional help. Being aware of warning signs and maintaining a supportive environment is crucial for their emotional well-being and recovery.
Signs that indicate someone may need immediate intervention include expressing feelings of hopelessness, talking about self-harm, withdrawal from friends and activities, significant mood changes, and increased substance abuse. Recognizing these signs early can be crucial for timely support and potential crisis management.
Promoting hope and resilience involves fostering supportive communities, encouraging open conversations about mental health, and providing access to resources. Engaging in activities that enhance well-being and connecting with others can empower individuals, helping them navigate life's challenges while reinforcing a sense of purpose and belonging. Riaz Counseling is dedicated to fostering hope and resilience in individuals by providing tailored support and resources. Their approach emphasizes personal growth, community connections, and the development of coping strategies to empower people in overcoming challenges associated with mental health and well-being.
If you feel that you or someone you know, may benefit from therapy, please reach out to our office for a FREE 15 minute consultation: LINK
Stay informed about the latest research in psychology.
.png)
Explore how Internal Family Systems (IFS) therapy heals trauma and restores self-leadership.
.png)
Explore how Internal Family Systems (IFS) therapy heals trauma, anxiety, and inner conflict.
.png)
A practical guide to recognizing, preventing, and healing teacher burnout in Houston schools.