
Medical school is known for its demanding curriculum and relentless pressure, but an often-overlooked consequence is loneliness. Many students experience emotional distress due to intense isolation, academic burnout, and limited social interactions. These factors can significantly affect mental health, leading to anxiety, depression, and even suicidal ideation. Addressing loneliness in med school is critical, not just for individual well-being, but also for producing resilient healthcare professionals. This guide explores the scope, causes, and solutions for student loneliness in today’s medical education landscape.

The medical school journey brings unique emotional challenges. Feelings of loneliness are common and can be more severe than in the general population. Social isolation, negative emotions, and academic stress combine to create higher levels of loneliness, especially among young adults in the United States.
Recent studies using tools like the Maslach Burnout Inventory and data from Google Scholar show medical students report greater loneliness than peers in other fields. Regional and cultural factors may further shape prevalence, with longitudinal studies highlighting transition periods and sample size variations impacting results.
Loneliness in medical education isn’t simply a lack of company. It’s a complex emotional state, characterized by persistent negative emotions and feelings of isolation, even in the midst of classmates and faculty. Emotional distress often emerges during periods of intense stress, as students grapple with high expectations and perfectionism.
The relationship between loneliness, academic burnout, and perceived stress is well documented. The current study reveals a strong correlation—loneliness feeds academic burnout, amplifying perceived stress, and vice versa. Medical students may face social isolation, limited meaningful social connections, and reduced empathy, all of which contribute to this cycle.
Social media offers only partial relief. While students connect virtually, real-life interactions are necessary for emotional support. The absence of deep, supportive relationships in medical school fosters emotional loneliness, making academic burnout and distress more likely. Addressing these issues is essential for student well-being.
Recent research on medical students in Houston, TX, reveals higher levels of loneliness than in many other academic disciplines. The data also connects loneliness with depressive symptoms and emotional distress.
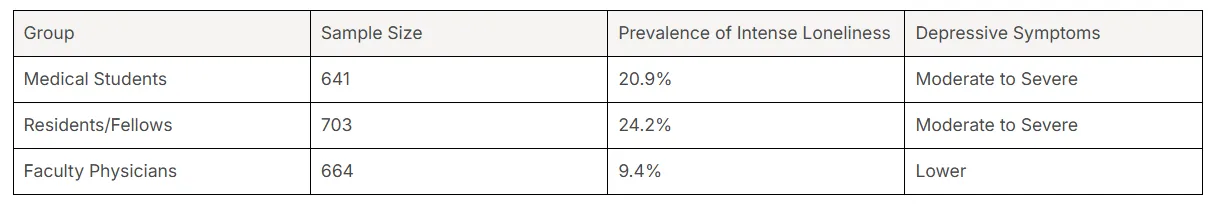
Medical students, especially those under 40, are at greater risk. Factors such as being female, non-White, or living in dormitories increase vulnerability. Compared to students in other fields, med students consistently report higher loneliness rates, pushing mental health issues to the forefront.
The relationship between loneliness and depressive symptoms is clear. Students who feel intensely lonely are more likely to experience moderate-to-severe depression, underscoring the need for targeted interventions in Houston and similar regions.
Medical students consistently report higher levels of loneliness than their peers in other academic fields. Social isolation and negative emotions are more prevalent, with longitudinal studies showing that these patterns persist over time. The general population experiences loneliness, but the rigors of medical education amplify this risk dramatically.
For example, cross-sectional research from Iran and Turkey found that the prevalence of loneliness among medical students was 26% to 60%, often surpassing rates found in other disciplines. Risk factors such as academic pressure, transition periods, and limited social interactions are more intense in medicine.
Loneliness is not only a matter of numbers; medical students also face deeper emotional distress. The necessity for meaningful social connections and constant exposure to high-stress environments makes their situation unique. This calls for specific strategies and support systems that address both academic demands and emotional needs.
Medical training is characterized by extreme academic pressure, long hours, and frequent relocations. These factors create barriers to social interaction, resulting in higher levels of loneliness compared to other students. The relentless demands leave little free time for meaningful social connections.
Social isolation, adjustment issues, and perfectionist expectations further compound the risk. Med school students face unique challenges, making them particularly susceptible to emotional distress and burnout. Next, let’s explore how workload, isolation, and transitions drive these problems and affect mental health.
The weight of academic expectations in medical school is a primary cause of loneliness. Intense workload, perfectionism, and continuous assessments using tools like the Maslach Burnout Inventory push students toward distress and mental health issues. The drive for excellence often leaves little room for rest or socializing.
Loneliness interacts with academic burnout and perceived stress, creating a cascade effect. Students experiencing emotional distress may withdraw from social interactions, and this isolation further reduces resilience. A recent study found that emotional loneliness and stress significantly increase the risk of burnout among medical students after the COVID-19 pandemic.
The negative emotions rooted in academic pressure undermine both mental health and academic performance. As the World Health Organization recognizes, burnout and distress are not just personal issues; they threaten the future of healthcare. Addressing perfectionism and workload is essential for breaking the cycle of loneliness.
Social isolation and a lack of free time are major contributors to loneliness among medical students. The demands of medical education—long hours, relentless study schedules, and frequent rotations—leave little opportunity for meaningful social connections. Social interactions are often superficial, limited to brief exchanges during lectures or clinical duties.
Effective strategies to cope with loneliness involve building structured support systems. Evidence shows that peer networks, campus activities, and group therapies offer emotional relief. For example, recurring meetings such as Schwartz Rounds foster empathy and support among classmates.
The relationship between loneliness, academic burnout, and perceived stress is cyclical. Without meaningful social connections, students are more susceptible to distress. Prioritizing time for real-life interactions and extracurricular activities can strengthen resilience and reduce negative emotions, breaking the isolation that so often defines medical school.
Transition periods—such as starting medical school, entering clinical years, or relocating for residency—pose significant risk factors for loneliness. Adjustment issues and emotional distress are common, especially among students who move away from family or familiar support systems.
Research highlights that first-year students and those relocating to new environments are at highest risk. Living in dormitories or confronting new academic cultures can intensify feelings of isolation. The shift to clinical years, with increased responsibilities and less peer contact, also elevates stress and loneliness.
Are there specific periods when loneliness peaks? Yes—transition phases, including exam seasons and rotations, see the highest vulnerability. Emotional bonds and resilience are tested, making institutional support and targeted interventions essential. Recognizing these high-risk times allows medical schools to implement timely programs that reduce adjustment difficulties and foster well-being.

Loneliness in medical school has serious consequences for both mental health and academic achievement. Students who experience prolonged isolation suffer increased burnout, distress, and depressive symptoms. These effects can escalate to anxiety, suicidal ideation, and long-term dissatisfaction in their medical careers.
Academic performance declines as motivation wanes and emotional distress rises. The cumulative impact of loneliness threatens both immediate success and future resilience for healthcare professionals. Exploring these effects in detail highlights the urgency of targeted solutions.
Medical students experiencing loneliness are at significantly greater risk for anxiety, depression, and burnout. Studies show that those reporting intense loneliness are much more likely to have moderate to severe depression (OR = 12.336) and heightened distress, as measured by the Maslach Burnout Inventory.
Burnout is not just emotional exhaustion—it’s a loss of empathy, increased callousness, and a sense of being emotionally drained. Lonely students exhibit more negative emotions, including irritability, nervousness, and feelings of being out of control. As Dr. Catherine Keiner notes, “Loneliness is a red flag for underlying depression and a modifiable risk for burnout, depression, and suicide risk.”
This persistent emotional distress impacts not only mental health but also the ability to cope with academic and professional challenges. Addressing loneliness is crucial for preventing these severe outcomes and supporting student resilience.
Loneliness directly undermines academic achievement and motivation. Students overwhelmed by negative emotions and emotional distress are less likely to engage actively with their studies. Depressive symptoms reduce cognitive performance, concentration, and self-efficacy.
Evidence indicates that loneliness and perceived stress mediate academic burnout. Emotional loneliness, more than social isolation, disrupts motivation and leads to lower academic satisfaction. The current study found that perceived stress is the strongest predictor of academic burnout, with emotional loneliness further amplifying its effects.
Is academic performance affected? Absolutely. Students facing persistent loneliness often procrastinate, struggle with perfectionism, and lose sight of their career goals. “Stress and loneliness increase academic burnout,” writes Cem Malakcioglu. Interventions focused on boosting emotional support and providing counseling can help reinvigorate motivation and restore balance.
Loneliness doesn’t just harm students now—it impacts long-term well-being and career satisfaction as future doctors. Chronic emotional distress erodes resilience, making healthcare professionals vulnerable to continued burnout throughout their careers.
Longitudinal studies confirm that those who experience intense loneliness as students report lower levels of job satisfaction and greater risk of depression and suicidal ideation as practicing physicians. Social isolation and negative emotions, if unaddressed, persist into residency and beyond, affecting work-life balance and relationships.
For example, trainees who lacked meaningful social connections during med school often struggle to form supportive professional networks. Institutional interventions, peer support groups, and routine social events are vital for building resilience. “Maximizing meaningful social connections within the hospital culture can minimize loneliness and reduce the risk of burnout and suicide,” emphasizes Sidney Zisook.
Certain phases in medical education present higher risks for loneliness. Preclinical years, clinical rotations, exam seasons, and the start of residency are particularly challenging. During these periods, students and trainees face increased academic demands, frequent transitions, and limited social interactions.
Understanding when loneliness peaks can guide targeted interventions. By identifying these high-risk times, medical schools can provide effective support, foster resilience, and help students form meaningful social connections that protect against emotional distress.
Loneliness shifts during the transition from preclinical to clinical years. In the preclinical phase, students experience more social isolation due to limited face-to-face interactions and reliance on virtual platforms. Emotional loneliness may be less pronounced, but social loneliness is higher, especially for those living away from family.
Clinical years bring increased exposure to stressful hospital environments and higher workloads. Emotional loneliness rises as students face greater psychological stress and reduced opportunities for peer bonding. The current study’s sample size demonstrates significant differences in loneliness between these groups, with clinical students more likely to feel emotionally isolated.
Are certain years more vulnerable? Yes—early clinical years, where students adjust to new roles and environments, are critical. Addressing loneliness during these transitions can prevent burnout and support students in building resilient coping skills.
Periods of intense academic assessment, such as exam seasons and clinical rotations, heighten negative emotions and distress among medical students. The pressure to excel and the demands of frequent evaluations create a climate of anxiety and emotional isolation.
Resilience is tested as students manage limited social interactions and high workloads. During rotations, shifts in group dynamics can disrupt established support networks, making meaningful social connections harder to maintain. A recent study found that perceived stress nearly doubled across terms, illustrating the cumulative impact of these high-pressure phases.
Are strategies available? Yes—evidence-based approaches such as peer support meetings and campus wellness activities can buffer the effects of exam seasons. Recognizing these vulnerable periods allows institutions to target resources, helping students navigate the challenges and minimize the risk of distress and academic burnout.
The start of residency is a high-risk period for loneliness. Trainees face new work environments, adjustment challenges, and demanding expectations. Mental health issues—anxiety, depression, and burnout—are especially prevalent in this phase, as higher levels of loneliness coincide with reduced social support.
Living in unfamiliar cities and working long hours exacerbate emotional distress. Trainees are often separated from previous peer networks, losing established sources of empathy and support. This transition can significantly impact resilience and well-being.
Are specific interventions needed? Absolutely. Early residency programs should emphasize social connection, mentorship, and accessible wellness resources. Addressing adjustment issues and building supportive communities at this stage can reduce vulnerability and improve both mental health and career satisfaction for healthcare professionals.

Tackling loneliness in medical school requires evidence-based strategies. Building supportive peer networks, engaging in campus activities, and seeking counseling are proven approaches for fostering meaningful social connections. Medical schools increasingly offer wellness resources and support programs to address these needs.
Students benefit most from interventions that prioritize empathy, group therapy, and structured extracurriculars. By leveraging campus initiatives, professional counseling, and peer support, med students can reduce negative emotions and strengthen their resilience against isolation and burnout.
Forming strong social connections with classmates and colleagues is among the most effective strategies to reduce loneliness. Peer networks provide empathy, support, and opportunities for genuine interaction, counteracting emotional distress and isolation.
Evidence shows that students who build robust peer networks experience less burnout and greater resilience. These connections foster meaningful social interactions, helping students navigate academic pressure and personal challenges. Supportive environments also enhance empathy and build lasting professional relationships.
Involvement in campus activities and interest groups is a powerful way to combat loneliness. Extracurriculars offer opportunities for meaningful social connections and diverse social interactions beyond the classroom.
These activities provide emotional support and foster a sense of belonging. Research confirms that engagement in campus communities boosts resilience and reduces negative emotions. By prioritizing extracurricular involvement, medical students can minimize social isolation and enhance overall well-being.
Professional counseling and access to wellness resources are essential for students facing intense loneliness. Medical schools increasingly offer confidential, secure services to help students manage distress and sensitive information.
Students who access counseling and wellness resources experience improved mental health and reduced burnout. These services offer tailored support, helping students process emotional distress and develop effective coping strategies. Institutional efforts to promote counseling ensure that every student can safely seek help without stigma or fear.
Medical schools play a crucial role in reducing loneliness through institutional support and local initiatives. Programs tailored to regional differences and cultural considerations ensure that interventions are relevant and effective. Houston medical schools, for example, have developed support systems that reflect the needs of their diverse student population.
Collaboration with local organizations and gov websites enhances these efforts. By prioritizing student wellness, campuses can promote resilience, foster meaningful connections, and address loneliness in culturally sensitive ways.
Houston medical schools are proactive in offering institutional support for student loneliness. Their programs are designed to address the unique risk factors faced by medical students and trainees.
Sample size data from Houston shows that students benefit from tailored interventions and accessible support systems. These programs foster empathy, reduce burnout, and address depressive symptoms. Ongoing evaluation and adaptation are key, ensuring that institutional efforts remain relevant for all students.
Regional differences and cultural considerations shape the prevalence and experience of loneliness among medical students. In the United States, factors such as race, gender, and economic status influence risk profiles. For instance, non-White and female students report higher levels of loneliness due to structural inequities and societal expectations.
Local initiatives must account for these variations. Programs in Houston and other regions adapt strategies to reflect cultural norms and community values. This includes providing targeted support for dormitory residents, international students, and those facing economic challenges.
Are there cultural differences in loneliness? Yes—studies show that the degree of autonomy, family relationships, and social stigma vary by region. Effective interventions require sensitivity to these factors. By customizing support programs, medical schools can better address the root causes of loneliness and promote psychological resilience for all students.
In summary, tackling loneliness in medical students requires a multifaceted approach. By understanding the unique challenges faced during medical training, students can take proactive steps to foster connections and seek support. Building peer networks, participating in campus activities, and accessing wellness resources are essential strategies to combat feelings of isolation. Additionally, medical schools play a crucial role by providing institutional support and promoting initiatives tailored to the needs of their students. It’s vital for medical students to prioritize their mental health and well-being, not just for their academic success, but for a fulfilling career ahead. For those seeking guidance, consider reaching out for a consultation to explore effective mental health resources tailored to your needs.
Riaz Counseling is one of the best top-rated counseling centers in Houston for cognitive behavioral therapy. These centers specialize in treating anxiety and depression, providing effective strategies to help students manage their mental health.
Riaz Counseling offers evidence-based treatment, including cognitive behavioral therapy for depression and anxiety. Their clinic is known for personalized care, utilizing proven therapeutic approaches to support students’ mental health and emotional well-being effectively.
Riaz Counseling accepts insurance from providers including BCBSTX, Optum, Magellan, Aetna, Cigna, and several others. Students can verify coverage securely through their official website or by contacting the clinic directly for specific healthcare professionals and options.
Many medical students have shared personal stories reflecting emotional distress and isolation during their training. Testimonials highlight challenges faced during transition periods, academic burnout, and the impact of meaningful social connections on overcoming loneliness in med school.
Balancing academics and social life requires strategic time management, prioritizing meaningful social interactions, and engaging in campus activities. Joining study groups, attending wellness workshops, and seeking peer support are proven ways for medical students to reduce loneliness and strengthen resilience.
Cultural differences significantly influence how medical students in the United States experience loneliness. Factors such as ethnicity, family values, and community support systems shape their perceptions and coping mechanisms, resulting in varied emotional responses to isolation and stress during their rigorous training.
If you feel that you or someone you know, may benefit from therapy, please reach out to our office for a FREE 15 minute consultation: LINK
Stay informed about the latest research in psychology.
.png)
Explore how Internal Family Systems (IFS) therapy heals trauma and restores self-leadership.
.png)
Explore how Internal Family Systems (IFS) therapy heals trauma, anxiety, and inner conflict.
.png)
A practical guide to recognizing, preventing, and healing teacher burnout in Houston schools.